
Dr. Subhas Gupta is the Chairman of the Department of Plastic Surgery at Loma Linda University in Southern California where he holds the academic rank of Professor and is the director of research. He is an innovative plastic surgeon who holds a PhD in Medical Informatics focused on the introduction of new technologies to clinical care. Dr. Gupta is the director of the Loma Linda University Soft Tissue Reconstruction Team and directs a bio-investigative cell biology and wound healing laboratory. Dr. Gupta is a paid consultant for 3M.
Gupta_Current-Dialogues-in-Wound-Management_2022_Article-3
Wound reconstructive surgical procedures are often indicated for complex wounds in all anatomic regions. These are major surgical interventions associated with a significant postoperative decline in functional capacity.1 Additionally, these procedures carry significant risks and have associated morbidity. Over the last three years, there has been increased attention given to the preoperative preparation of surgical patients with the goal of enhancing their recovery. The concept of Enhanced Recovery After Surgery (ERAS) has received much attention, but little focus has been directed to preoperative optimization of these same patients. Our advanced reconstructive plastic surgery practice has developed a pathway of preoperative patient preparation designed to enhance patients’ functional capacity at baseline, in addition to an ERAS protocol instituted postoperatively. Our center has found that this allows patients to return to their baseline function more rapidly. Perhaps more importantly, it may lower the rate of complications, including surgical site infection.
Background
Preoperative patient optimization, termed ‘prehabilitation’, is defined as a series of activities designed to enhance an individual’s functional capacity to enable the withstanding of a forthcoming stressor, such as major surgery. Most prehabilitation programs incorporate a multimodal approach, including medical optimization, preoperative physical exercise, nutritional support, and stress/anxiety reduction.2
The first major article on prehabilitation was published in 2014 in a colorectal surgery patient population.3 The authors presented an overview of a concept of making patients fit for surgery before they had surgery. The focus of the study was on three main parameters: worry, nutrition, and exercise. A significant effort was spent on alleviating preoperative anxiety and stress. The authors also focused on enhancing protein intake, protein absorption, and increasing the preoperative functional capacity of patients. Consequently, when the patients underwent surgery, their decrease in functional capacity was not as significant as patients who did not undergo the prehabilitation protocol.3
Additional authors have since reported other methods of prehabilitation.4,5 These all tend to revolve around patient empowerment, behavior modification, and improved outcomes. Numerous studies have shown that hospital length of stay has been reduced, healthcare costs have been lowered, and most importantly, patients have achieved better outcomes and fewer complications when initiated into a well-implemented prehabilitation program.
Loma Linda University Prehabilitation Program
At our center, surgical prehabilitation occurs as the time between the decision to perform surgery and the beginning of acute surgical care. The prehabilitation program includes physical and psychological assessments that establish a baseline functional level, identify impairments, and provide interventions that promote physical and psychological health to reduce the incidence and/or severity of future impairment. Our prehabilitation program was developed with the following goals:
- Improving cardiovascular, pulmonary, and/or musculoskeletal function.
- Improving balance to reduce the risk of falls.
- Reducing anxiety and improve coping with specific cognitive behavioral strategies.
- Improving quality of sleep with sleep hygiene education.
- Optimizing surgical outcomes with smoking cessation interventions.
- Optimizing diet with nutrition counseling.
- Educating around postoperative routines to prepare a safe home environment.
- The medical optimization portion focuses on assessing and improving the following underlying comorbidities:
- Anemia correction
- Glycemic control with a hemoglobin A1C < 7.5
- Blood pressure control
- Smoking cessation
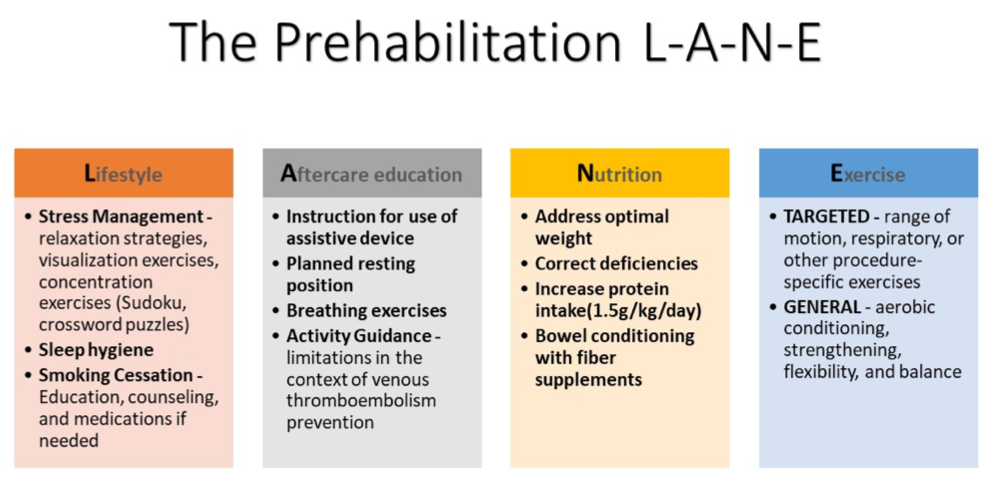
While medical optimization is occurring, patients are provided education and counseling that focus on four key pillars that have been coined the prehabilitation LANE (Figure 1).
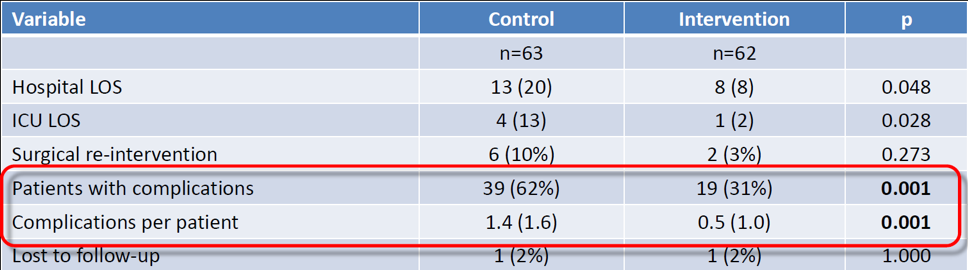
In an observational cohort of 125 patients (62 patients compared to a 63-patient historical control) at our institution, the prehabilitation protocol demonstrated statistically significant reductions in complications and improved overall satisfaction in patients undergoing major procedures. In addition, hospital length of stay and intensive care unit length of stay were also significantly reduced in the prehabilitation group compared with the control group. Surgical re-interventions were also reduced but were not statistically significant. Key data outcomes are summarized in Table 1 below.
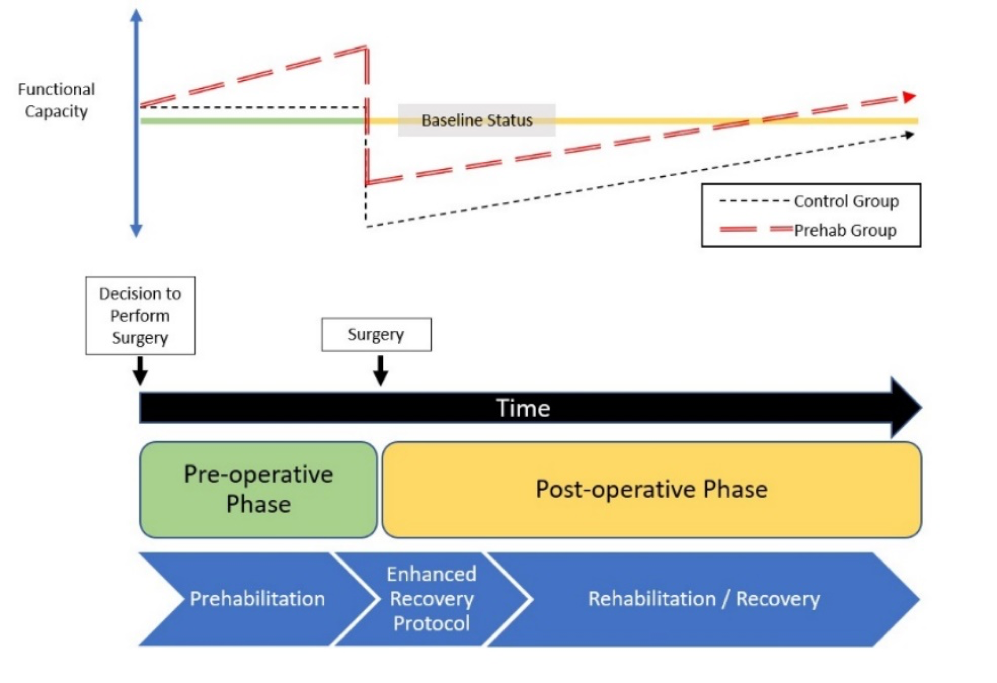
Our single center experience suggests that implementing a surgical prehabilitation program that focuses on the four categories of exercise or functional capacity evaluation and optimization, psychological intervention (focused on relaxation and sleeping techniques), nutritional intervention (protein supplementation up to 1.5 grams per kilogram per day with some specific immunonutrition, including arginine) and medical optimization (anemia correction, glycemic and blood pressure control, and smoking cessation) can provide improved outcomes for patients undergoing major surgical procedures. Conceptually, if the patient undergoes prehabilitation, functional capacity may increase before surgery (Figure 2). While there was almost certainly an increase in preoperative functional capacity in our study cohort, this was not discretely measured. As has been well established with ERAS protocols, a more rapid return to functional capacity after surgery is considered a major factor in complication reduction. With the incorporation of prehabilitation, the patient’s preoperative functional capacity is increased, which suggests that the physiologic impact of surgery is attenuated, resulting in a higher postoperative capacity and a quicker return to baseline capacity.
Implementation in Practice and “EPRAS”
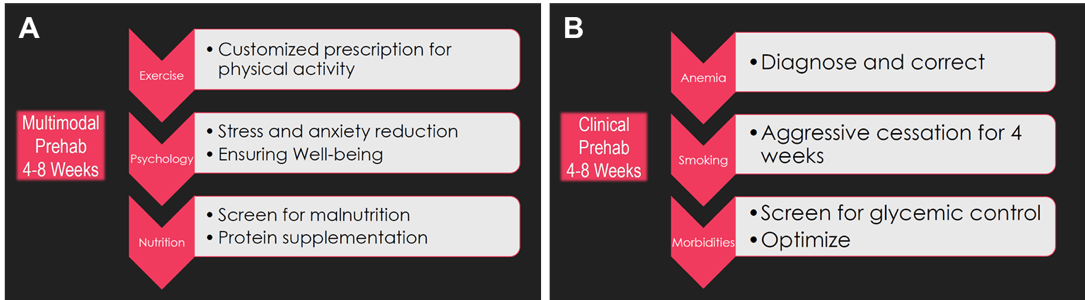
To summarize the components of prehabilitation into an implementation paradigm, we have divided the interventions into two groups that should be delivered concurrently to the patient. Ideally, to achieve a significant improvement in functional capacity, multimodal prehabilitation should occur anywhere from four to eight weeks before surgery. The prehabilitation LANE components of lifestyle, aftercare education, nutrition, and exercise instruction should occur once the decision to perform surgery has been made. Simultaneously, a clinical path of assessment and correction of anemia, aggressive smoking cessation, and enhancement of glycemic and blood pressure control should be initiated for at least four weeks (Figure 3).
Many clinical improvements have resulted from the recent developments in ERAS protocols. To optimize the outcomes of surgical wound reconstruction patients, we propose the “EPRAS method”: Enhanced Prehabilitation and Recovery After Surgery. Optimally, patients undergoing scheduled surgical procedures will undergo both a prehabilitation program to enhance their functional capacity at baseline and then undergo an enhanced recovery after surgery protocol following surgery. This may facilitate a much more rapid return to their baseline function and lower rates of complications, including reducing and preventing surgical site infection.
References
- McMath, K., Gupta, S. A Novel Prehabilitation Protocol: Improving Outcomes and Reducing Morbidity in a Complex Surgical Wound Population. Wound Healing Society 2022 Annual Meeting; April 6-10,2022; Phoenix, AZ.
- Hamlin MJ, Yule E, Elliot CA, Stoner L, Kathiravel Y. Long-term effectiveness of the New Zealand Green Prescription primary health care exercise initiative. Public Health. 2016;140:102-108. doi:10.1016/j.puhe.2016.07.014
- Gillis C, Li C, Lee L, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014;121(5):937-947. doi:10.1097/ALN.0000000000000393
- Tew GA, Ayyash R, Durrand J, Danjoux GR. Clinical guideline and recommendations on pre-operative exercise training in patients awaiting major non-cardiac surgery. Anaesthesia. 2018;73(6):750-768. doi:10.1111/anae.14177
- West MA, Wischmeyer PE, Grocott MPW. Prehabilitation and Nutritional Support to Improve Perioperative Outcomes. Curr Anesthesiol Rep. 2017;7(4):340-349. doi:10.1007/s40140-017-0245-2\
Figures courtesy of Subhas Gupta, MD, CM, PhD, FRCSC, FACS.
©2022 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. 3M Marks used under license in Canada.

