Dr. Orgill is Vice Chairman for Quality Improvement in the Department of Surgery at Brigham and Women’s Hospital and Professor of Surgery at Harvard Medical School. He is a reconstructive plastic surgeon and has a PhD from MIT in Medical Engineering. He is the Director of the Brigham and Women’s Hospital Wound Care Center and runs a tissue engineering and wound healing Laboratory. His lab at BWH is working to develop better technologies to treat wounds including work with artificial skin, micromechanical forces, platelets and stem cells. He has consulted for several medical device and start-up companies and is the inventor on several patents. He worked on the team that developed Integra, a skin replacement therapy that has been commercially developed and used successfully on thousands of patients. Dr. Orgill is a paid consultant for 3M.
Orgill_Current-Dialogues-in-Wound-Management_2022_Article-5
INTRODUCTION
Open heart surgery has prolonged millions of lives but is one of the most invasive surgical procedures performed today. In most cases, patients are placed on cardio-pulmonary bypass to allow surgeons to work on a heart that is not beating. Common operations include coronary bypass grafting and heart valve repair or replacement. Sternal wound infections can be one of the most dreaded complications in all of surgery. Patients can develop mediastinitis, which if not promptly treated, can quickly lead to sepsis and death. In some cases, the infectious process can erode into large vascular structures and cause exsanguination. In our institution, we have worked diligently to reduce the incidence of sternal wound infections while improving techniques to treat them.1
Reducing the number of patients requiring open-heart surgery
A revolution has occurred in minimally invasive cardiac procedures for coronary artery disease which includes a variety of angioplasty techniques and stent procedures. Over the last 14 years, coronary artery bypass grafting in North America has decreased by over 23% to just over 200,000 cases per year in 2021.2 This is in the setting of an aging population with increases in diabetes and obesity. Although cardiac stenting procedures have been slowly growing, there is emerging evidence that comparable outcomes can be achieved in patients with stable disease with good medical management as compared to an initial invasive strategy.3 Transcatheter aortic valve replacements (TAVR) have grown substantially since first being approved by the FDA in 2011 and in 2019 close to 80,000 TAVRs were performed compared to about 58,000 surgical replacements.4
Reducing the percentage of patients who develop sternal wound infections
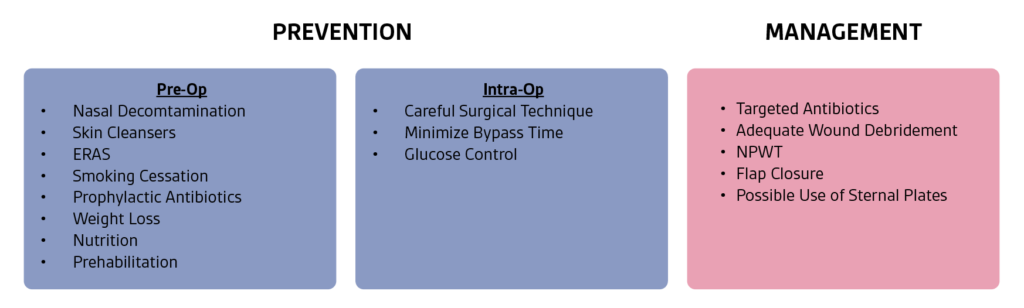
There are several measures that surgeons can use pre-operatively to reduce the risk of sternal wound complications including smoking cessation, optimization of nutrition and weight loss. We share several strategies listed below that have been closely studied.
Nasal decontamination
Strong evidence exists for the use of pre-operative nasal ointment administration in patients with Staphylococcus nasal colonization in the absence of PCR testing or nasal cultures positive for staphylococcal colonization.5 Empiric studies have shown that when sternal isolates occur, they match colonization of the nose.
Pre-operative Antibiotics
First generation cephalosporin antibiotics are standard of care and should be administered before the incision is performed. Ideally, the intravenous administration of a cephalosporin antibiotic should occur within 60 min of the surgical procedure, continue for procedures of more than 4 hours, and not used for more than 48 hours. The dosing should be weight based. Vancomycin can be administered in patients where methicillin-resistant Staphylococcus aureus may be of concern on pre‑operative nasal cultures or for patients that are allergic to cephalosporin.5 The pre-operative antibiotic regimen may differ between clinical settings depending on the microbiological profile of the institution.
Peri-operative Glycemic Control
Achieving hemoglobin A1c levels at ≤ 7.5% pre-operatively has also been shown to reduce post-operative infection. In our institution, we aim for post-operative glucose levels < 180 mg/dL in the peri-operative period. Multiple published studies have demonstrated that increased glucose levels (>200 mg/dL) in the intraoperative period is an independent risk factor for postoperative sternal wound infections. Additionally, studies have shown that maintaining serum glucose level <180 mg/dL during surgery significantly decreases the incidence of sternal wound infections. This is best done with a continuous insulin infusion.5
Other methods to minimize the risk of sternal wound infection
There have been several other methods that many cardiac surgeons adhere to including smoking cessation in advance of the surgery, weight loss, when possible, nutritional optimization, prehabilitation6 and pre-operative skin cleansing. Many centers are now using the principles of enhanced recovery after surgery (ERAS) to improve outcomes following surgery. ERAS is a multimodal, transdisciplinary care improvement initiative to promote recovery of patients undergoing surgery throughout their entire perioperative journey. One retrospective analysis of an institution’s coronary artery bypass graft database using an ERAS approach demonstrated reduced total and postoperative length-of-stay (LOS), reduced total ventilation time, and increased early extubation for all 1,079 patients.7 Surgical technique also likely contributes to the risk of sternal wound infection, including the judicious use of the electrocautery, making sure the sternotomy is in the center of the sternum and minimizing prolonged bypass times.
Sternal stabilization techniques
Rigid fixation has several theoretical advantages and may be useful prophylactically in certain high-risk individuals for sternal wound infection and in the treatment of sternal complications.8 These devices are expensive, require additional dissection of the sternum and if they do become infected often require a large-scale debridement of bone. If plates are used, the cardiac surgeons need to be familiar with how to rapidly remove them should they need to rapidly expose the heart during a post-operative emergency. More studies in this area will be needed to clarify which patients may benefit from this technology.
Better Management of Sternal Wound Infections
Patient care for sternal wound infection requires treatment of infection using appropriate institutional practices (i.e., use of targeted antibiotic therapy) along with wound management. Sternal wound management can include surgical debridement, negative pressure wound therapy (NPWT) use, wound closure, and sternal stabilization
NPWT devices have dramatically changed the way that we manage sternal wound at our institution. For patients with an unstable sternum, continuous NPWT has been recommended throughout the treatment period to help stabilize the chest wall. NPWT helps pull the wound edges together and provides a “splinting” effect, which may allow the patient to be more mobile and comfortable. In our institution, use of NPWT to manage the sternal wound in patients with an acute sternal infection helps provide a method to stabilize the sternum that allows most patients to be taken off the ventilator and to ambulate so that the reconstructive procedure can be carried out semi-electively. Practically speaking, if a patient develops surgical site complications in the middle of the night or over a weekend, they can be taken to the operating room for a simple washout procedure and placement of a NPWT device. There have been anecdotal reports of severe bleeding if the open pore polyurethane sponge is placed directly over the right ventricle or over the coronary artery bypass graft. Manufacturers of NPWT warn of the potential for bleeding complications in the instructions for use. Care should be taken when NPWT is used in patients who have weakened or friable blood vessels or organs in or around the wound, are without adequate wound hemostasis, have been administered anticoagulants or platelet aggregation inhibitors, or do not have adequate tissue coverage over vascular structures as NPWT is not used to prevent, minimize, or stop vascular bleeding. To obviate the risk for bleeding complications, surgeons may use a thick layer of natural tissue or consider placing a non-adherent material as an alternative over these vascularized structures to minimize the risk of erosion. If using non-adherent materials, ensure they are secured in a manner that will maintain their protective position throughout therapy. If NPWT is prescribed for patients who have an increased risk of bleeding complications, they should be treated and monitored in a care setting deemed appropriate by the treating physician.
For patients with chronic infections, our institution often uses NPWT devices over sternal wires, to help pull the wound edges together and provide a “splinting” effect, and will wait for osteosynthesis to occur before removing bone fixation materials while the patient is being treated for infection using infection management protocols. It is considered best practice to keep patients in the hospital if a NPWT device is used without the sternum being closed.
Cross-disciplinary management with colleagues from infectious disease helps in determining if long-term antibiotics are needed. To treat possible osteomyelitis, a course of antibiotic therapy for several weeks may be required. The trend has been to treat more patients with antibiotics by mouth and for shorter time periods.9
Flaps
Flaps have revolutionized sternal reconstruction by bringing in vascularized tissue to fill dead spaces and deliver antibiotics to infected tissues. In the majority of flap procedures, the pectoralis major myocutaneous advancement flaps provide excellent coverage while eliminating dead space and providing sternal compression. Evidence has shown that secondary flap options, such as the omental flap or rectus abdominis muscle, may occasionally be necessary.10 Reconstruction can be based on either the thoracoacromial trunk or based on mammary perforators. Note that in patients that have had their internal mammary artery harvested for a bypass graft, the mammary perforators may not provide adequate blood flow. We frequently observe this on the left side and often observe that both the bone and soft tissues have less blood supply compared with the right side.
The omentum provides a large flap with excellent vascularity. It can be harvested through the diaphragm, often without extending the sternotomy incision and has been associated with faster operating time and less blood loss as compared with a laparotomy incision.11
Sternal Preservation
For infected sternums, particularly in younger individuals, there are advantages to achieving sternal union. In these individuals, movement of the sternal tables against each other can cause pain and discomfort. There can be some paradoxical movement with breathing. Sternal preservation can be achieved with re-wiring or sternal plating techniques.
Conclusions
The complications following cardiac surgery have substantially decreased over the last several years. One large reason is the reduction in open cardiac surgical procedures with treatment paradigms moving towards minimally invasive techniques and better medical therapies for heart disease. Improvement in therapies such as pre-operative antibiotics, glucose control and nasal decontamination have also helped improve surgical outcomes (Figure 1). Finally, having a team of reconstructive surgeons with good availability to perform flap closure can help minimize the risk of complications when patients have sternal wound infections.
References
- Matros E, Aranki SF, Bayer LR, McGurk S, Neuwalder J, Orgill DP. Reduction in incidence of deep sternal wound infections: random or real?. J Thorac Cardiovasc Surg. 2010;139(3):680-685.
- Statista Research Department. Number of North American cardiovascular surgeries 2007-2021. https://www.statista.com/statistics/647958/cardiovascular-surgery-north-america-numbers/. Accessed July 2022
- Maron DJ, Hochman JS, Reynolds HR, et al. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N Engl J Med. 2020;382(15):1395-1407.
- Report finds TAVR is dominant form of aortic valve replacement, outcomes steadily improving in the United States [press release]. Washington DC: American College of Cardiology; November 16, 2020. https://www.acc.org/about-acc/press-releases/2020/11/16/18/53/report-finds-tavr-is-dominant-form-of-aortic-valve-replacement-outcomes-steadily-improving-in-the-us. Accessed July 2022.
- Lazar HL, Salm TV, Engelman R, Orgill D, Gordon S. Prevention and management of sternal wound infections. J Thorac Cardiovasc Surg. 2016;152(4):962-972.
- Rouleau CR, Chirico D, Hauer T, Kidd W, Arena R, Aggarwal SG. An observational study examining utilization of prehabilitation and its association with postoperative cardiac rehabilitation participation and risk factors following coronary artery bypass grafting. Int J Cardiol. 2022;362:28-34.
- Sutton TS, McKay RG, Mather J, et al. Enhanced Recovery After Surgery Is Associated With Improved Outcomes and Reduced Racial and Ethnic Disparities After Isolated Coronary Artery Bypass Surgery: A Retrospective Analysis With Propensity-Score Matching. J Cardiothorac Vasc Anesth. 2022;36(8 Pt A):2418-2431.
- Liao JM, Chan P, Cornwell L, et al. Feasibility of primary sternal plating for morbidly obese patients after cardiac surgery. J Cardiothorac Surg. 2019;14(1):25.
- Hamaguchi R, Shekar PS, Johnson JA, Orgill DP. Current Management of Sternal Wounds. Plast Reconstr Surg. 2021;148(6):1012e-1025e.
- Levy AS, Ascherman JA. Sternal Wound Reconstruction Made Simple. Plast Reconstr Surg Glob Open. 2019;7(11):e2488.
- Vyas RM, Prsic A, Orgill DP. Transdiaphragmatic omental harvest: a simple, efficient method for sternal wound coverage. Plast Reconstr Surg. 2013;131(3):544-552.
NOTE: Specific indications, contraindications, warnings, precautions and safety information exist for these products and therapies, some of which may be Rx only. Please consult a clinician and product instructions for use prior to application.
©2022 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. Used under license in Canada.

