Christopher Mantyh is the Chief of Colorectal Surgery and Professor of Surgery at Duke University Medical Center. He has recently been named as the Chief of Quality for the Department of Surgery. Dr. Mantyh has implemented changes to improve best practices in surgical procedures performed at Duke Hospital using multiple platforms including the National Surgical Quality Improvement Project, for which he is the Surgical Champion. In that role, he has championed a quality improvement plan based on the surgical bundles and Early Recovery After Surgery (ERAS) protocol that has led to significant improvements in clinical patient outcomes and cost savings. In addition, his research over the last five years has been focused on quality indexes and outcomes in colorectal cancer. His multi-disciplinary work has spanned the spectrum of treatment of colorectal cancer from novel endoscopic imaging of colonic dysplasia, to proper operative technique, and evaluation of molecular markers of colorectal cancer to help determine individualized chemotherapy. Collaborative efforts include working closely with bioengineering, radiation oncology, medical oncology, statisticians, and physiologists. Recently, his group has investigated large national databases to develop predictive modeling systems to anticipate surgical complications. He is currently funded through multiple foundation and national grants. He has over 130 peer reviewed publications and book chapters.

Dr. Megan Turner is a third-year general surgery resident at Duke University in Durham, North Carolina. She went to medical school at the University of Washington in Seattle. Her academic interests include perioperative decision making, behavioral economics, gender in the workplace, and outcomes research.
Mantyh and Turner_The Chronicles of Incision Management_2017_Volume 1_Issue 1
Background
Increasing emphasis on hospital performance has led to the collection and analysis of data used to interpret and improve the quality and cost of care for patients. One of the most important quality metrics for surgical departments is the rate of postoperative surgical site infection (SSI). Hospital-acquired infections affect 440,000 patients, with one fifth attributed to SSI, and at cost $9.8 billion annually. One third of this cost is attributable to SSI.1, 2 The impact of SSI on overall morbidity and mortality for patients undergoing operations is substantial, and now inextricably linked to performance ranking and reimbursement.3, 4 Given the additive interests of improving patient outcomes and economic incentives, several mechanisms for improving SSI rates have been proposed and subsequently analyzed for cost effectiveness.
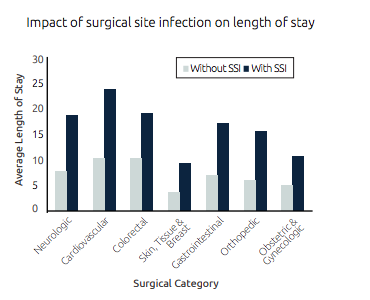
All operations portend some risk for surgical site infection. There are well-defined risk factors used to predict those who have disproportionate morbidity from SSI. Affected patients include those undergoing colorectal operations, emergency operations, open versus minimally invasive operations, patients undergoing chemotherapy, prior radiation, and those taking immunosuppression. The morbidity of SSI to patients is well understood. Both retrospective and prospective studies have examined the impact on recovery from major operations complicated by SSI, independent of the patient’s comorbidities.6-11Patients experiencing SSI have increased length of stay, increased readmission rates, longer delays in return to work, and lower satisfaction with care.
Costs Attributable to Surgical Site Infections
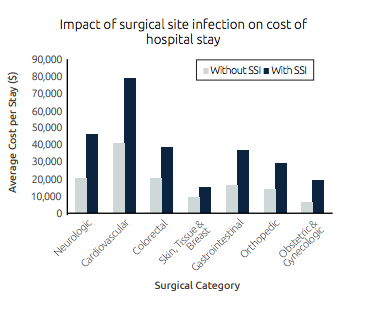
The true cost of SSI is difficult to quantify given variations in methodology utilizing variable intrinsic and extrinsic costs. National estimates reach over $3 billion dollars annually.2, 12 Intrinsic costs of SSI to patient care are in the management of the infection: additional operations, procedures, nursing, wound management personnel time, infectious disease interventions, loss of time from work, and costs associated with home health.11 Extrinsic costs are substantial, including the reputation of the medical center and the impact of variable reimbursement and penalties based on performance. In 2013, Zimlichman et al. estimated the additional cost of SSI to be $20,785 (95% CI $18,902 – $22,667) per occurrence.2 This is comparable to estimates by de Lissovoy, $20,842 in 2009.
With increased public attention to preventable harm in the hospital setting (following the 1999 publication To Err is Human) a development of quality initiatives has garnered national support. Preventable SSI for surgical patients became increasingly scrutinized. Metrics were developed for institutional monitoring and public reporting of SSI. These programs include National Healthcare Safety Network (NHSN), Agency for Healthcare Research and Quality Patient Safety Indicators (AHRQ PSI), and American College of Surgeons National Surgical Quality Improvement Project (NSQIP). While each program has different methods of data acquisition, monitoring within an institution can occur over time and comparisons can be made between institutions. The metrics serve as a mechanism to monitor the success of quality improvement processes.
In an attempt to improve postoperative outcomes, guidelines were developed by quality improvement groups. The 2002 Surgical Infection Prevention measures were developed and implemented, leading to the evolution of the Joint Commission best practice guidelines, updated in 2014.13 These guidelines are presented in the publication A Compendium of Strategies to Prevent Healthcare Associated Infections in Acute Care Hospitals and include parenteral preoperative antibiotics one hour prior to incision, antibiotics consistent with published guidelines, antibiotics discontinued within twenty-four hours of surgery, normothermia, standardization of skin preparation and patient and family education.13 The Joint Commission Center for Transforming Health Care reported a 32% reduction in SSI, and a savings of $3.7 million following implementation of their guidelines.
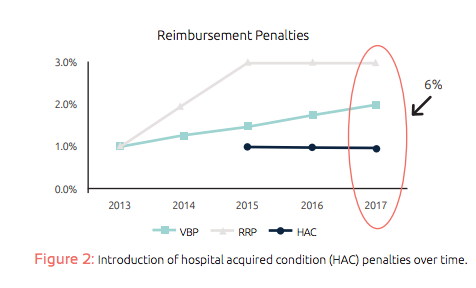
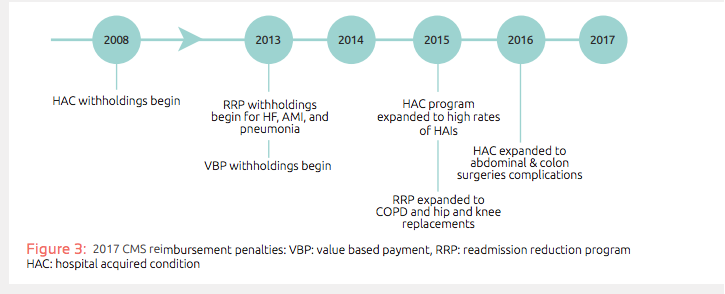
In 2007, the Center for Medicare/Medicaid Services (CMS) developed penalty guidelines for non-reimbursement of several hospital-acquired conditions. The updated 2013 guidelines included SSI following coronary artery bypass grafting, bariatric surgery, designated orthopaedic operations, and implantable cardiac devices. In 2014, payment reductions were initiated for hospitals in the lowest performing quartiles for composite scores based on six quality measures: Central Line-Associated Bloodstream Infection (CLABSI), Catheter-Associated Urinary Tract Infection (CAUTI), Surgical Site Infection (SSI) (Colon Surgery and Abdominal Hysterectomy), Methicillin-resistant Staphylococcus aureus (MRSA) bacteremia, and Clostridium difficile Infection (CDI). Penalties through CMS may reach as high as 6% in 2017 (figure 3), an increase from prior penalties. Private insurers are predicted to follow suit with their reimbursement policies. Given that many hospitals operate at a 4-5% profit margin, the impact of SSI penalties may have significant consequences for these organizations.
Current Strategies for Prevention of SSI
Financial implications associated with impending CMS penalties require hospitals to take a systematic approach to SSI reduction. Nearly 55% of surgical site infections are deemed preventable.17 Guidelines have been developed to systematically reduce SSI with success. The past century of research has culminated in bundle implementation of multiple SSI prevention strategies. Institutions with higher than expected SSI rates have dramatically improved their SSI rates by obtaining quality metrics through NSQIP, NHSN, or AHRQ PSI and implementing quality improvement projects.
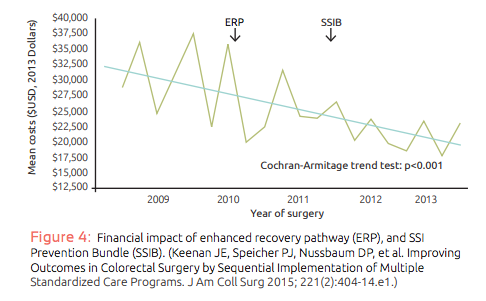
Several current mechanisms exist to promote better outcomes, demonstrate reduction in SSI rates, and are cost effective to implement. A single institution utilized their 30-day NSQIP data to compare SSI in colorectal surgical patients, following implementation of an enhanced recovery pathway, and a SSI prevention bundle. They found a reduction in infection rates and a reduction in overall cost for colorectal surgical admissions. Following implementation of an enhanced recovery pathway they saw a reduction in length of stay, which frequently is used as a cost surrogate. The implementation of the SSI prevention bundle decreased rates of superficial site infection (16.1% vs 6.3% p<0.01) and sepsis (11.2% vs 1.8% p <0.01). While some overhead costs exist in the implementation of such programs, overall cost for admissions can be reduced ($31,926 in 2008 vs $22,044 in 2013 p<0.01).18 This study expands on the previous efficacy study of bundled SSI prevention and enhanced recovery pathways.19-21 This experience demonstrates feasible, cost effective improvements in SSI rates with successful implementation of comprehensive perioperative pathways.
Conclusion
SSI is a widely utilized and appropriate metric for quality of surgical care that has complex economic implications that are difficult to quantify. CMS penalties for postoperative surgical site infection may reach as high as 6% in 2017. Private insurers are anticipated to follow suit. Many hospitals may find their financial stability at risk. Incentives to implement systems processes including enhanced recovery pathways and SSI bundles should be promoted to maximize prevention of surgical site infection.
References
1.Klevens RM, Edwards JR, Richards CL, Jr., et al. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep 2007; 122(2):160-6.
2.Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med 2013; 173(22):2039-46.
3.Dimick JB, Chen SL, Taheri PA, et al. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg 2004; 199(4):531-7.
4.Bratzler DW, Hunt DR. The surgical infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery. Clin Infect Dis 2006; 43(3):322-30.
5.McNair PD, Luft HS, Bindman AB. Medicare’s policy not to pay for treating hospital-acquired conditions: the impact. Health Aff (Millwood) 2009; 28(5):1485-93.
6.Schilling PL, Dimick JB, Birkmeyer JD. Prioritizing quality improvement in general surgery. J Am Coll Surg 2008; 207(5):698-704.
7.Merkow RP, Ju MH, Chung JW, et al. Underlying reasons associated with hospital readmission following surgery in the United States. Jama 2015; 313(5):483-95.
8.McCoy CC, Englum BR, Keenan JE, et al. Impact of specific postoperative complications on the outcomes of emergency general surgery patients. J Trauma Acute Care Surg 2015; 78(5):912-8; discussion 918-9.
9.de Lissovoy G, Fraeman K, Hutchins V, et al. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control 2009; 37(5):387-97.
10.Kirkland KB, Briggs JP, Trivette SL, et al. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol 1999; 20(11):725-30.
11.Wick EC, Hirose K, Shore AD, et al. Surgical site infections and cost in obese patients undergoing colorectal surgery. Arch Surg 2011; 146(9):1068-72.
12.Broex EC, van Asselt AD, Bruggeman CA, et al. Surgical site infections: how high are the costs? J Hosp Infect 2009; 72(3):193-201.
13.Yokoe DS, Anderson DJ, Berenholtz SM, et al. A compendium of strategies to prevent healthcare-associated infections in acute care hospitals: 2014 updates. Infect Control Hosp Epidemiol 2014; 35(8):967-77.
14.Care TJCCfTH. SSI Infographic. 2010.
15.Healthcare JCCfT. Reducing Colorectal Surgical Site Infections 2017. Available at: http://www.centerfortransforminghealthcare.org/assets/4/6/infographic_ssi.pdf.
16.Services CfMM. Hospital-Acquired Conditions. 2015.
17.Umscheid CA, Mitchell MD, Doshi JA, et al. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol 2011; 32(2):101-14.
18.Keenan JE, Speicher PJ, Nussbaum DP, et al. Improving Outcomes in Colorectal Surgery by Sequential Implementation of Multiple Standardized Care Programs. J Am Coll Surg 2015; 221(2):404-14.e1.
19.Hedrick TL, Heckman JA, Smith RL, et al. Efficacy of protocol implementation on incidence of wound infection in colorectal operations. J Am Coll Surg 2007; 205(3):432-8.
20.Lee L, Li C, Landry T, et al. A systematic review of economic evaluations of enhanced recovery pathways for colorectal surgery. Ann Surg 2014; 259(4):670-6.
21.Keenan JE, Speicher PJ, Thacker JK, et al. The preventive surgical site infection bundle in colorectal surgery: an effective approach to surgical site infection reduction and health care cost savings. JAMA Surg 2014; 149(10):1045-52.