
Dr. Robert Snyder is a podiatrist with over 30 years of experience; his practice is limited to wound management and limb preservation. He is Professor and Director of Clinical Research and Fellowship Director at Barry University SPM. Dr. Snyder is certified in foot and ankle surgery by the American Board of Podiatric Surgery and is also a board certified wound specialist. Dr. Snyder is immediate past-president of the Association for the Advancement of Wound Care and past-president of the American Board of Wound Management. In addition to his doctorate, he holds an MSc in Wound Healing and Tissue Repair from Cardiff University. Dr. Snyder has published several book chapters over 125 papers in peer reviewed and trade journals on wound care and has been a principal investigator on more than 30 randomized controlled trials.
Snyder_Current Dialogues in Wound Management_2016_Volume 2_Issue 2
Infected wounds in patients with diabetes represent the major reason why this patient demographic is hospitalized.1 Therefore, many patients present to the clinic with severe infections requiring in-patient interventions. During this event, the multidisciplinary model is utilized to help insure a comprehensive, evidence based and holistic approach to patient care.2 The Institute of Medicine purports that the cost and complexity of the team is directly proportional to a patient needs.3 (Fig 1) This team usually includes internal medicine, podiatry, vascular, and infectious disease as the “irreducible minimum.” Surgical intervention includes elective, palliative, and emergent scenarios. However, in many cases surgery is performed urgently to save limb and life. Among the many criteria for evaluating these patients, the Infectious Disease Society of America and International Working Group on the Diabetic Foot Classifications of Foot Infections (uninfected, mild, moderate, and severe) represents a pragmatic approach that may aid in diagnostic and ultimate treatment pathways.
Ideally, the patient should be thoroughly evaluated by the vascular team prior to surgical intervention; however, in emergent situations (i.e. gas in the tissue) surgery to drain infected areas and remove liquefactive necrosis is the first order of business. Postoperative or other interventions while hospitalized may include moist wound healing and management of dead space utilizing Negative Pressure Wound Therapy (NPWT) with instillation, among others. In many cases, the wound is left open for a period of time (i.e. 5-7 days) and subsequently closed with delayed primary closure. However, there are instances where the patient is discharged with an open
surgical wound (i.e. extensive tissue loss, continued infection) that may even be covered with cadaveric allograft material requiring meticulous attention on an outpatient basis.
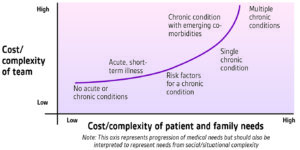 Figure 1. Cost versus complexity of a multidisciplinary team. Mitchell P, Wynia M, Golden R, et al. Core principles & values of effective team-based health care. Discussion Paper, Institute of Medicine. Washington, DC. 2012. www.iom.edu/tbc. Accessed [online] 24 April 2016
Figure 1. Cost versus complexity of a multidisciplinary team. Mitchell P, Wynia M, Golden R, et al. Core principles & values of effective team-based health care. Discussion Paper, Institute of Medicine. Washington, DC. 2012. www.iom.edu/tbc. Accessed [online] 24 April 2016
Sadly, once discharged, many patients are lost to follow-up; patient adherence represents a key to a successful outcome. Therefore, creating a continuum of care remains critical and should be planned with input from the hospital Case Manager in conjunction with all physicians involved in the care of the patient prior to discharge.5 (Fig 2) Many patients leave with PICC lines, and antibiotic therapy has to be organized, as well as hyperbaric oxygen treatments if required. Establishing home healthcare is often essential.
Upon discharge the patient should be managed utilizing the wound bed preparation model including addressing patient-centered concerns. Additionally, the ulcer should be approached with continued wound debridement as required, the management/ surveillance of infection, the maintenance of moist wound healing (i.e. foams, hydrogels, alginates, collagen-ORC, collagen-ORC with silver) while assuring the wound edge is
 Figure 2: The continuum of care model
Figure 2: The continuum of care model
appropriately addressed to facilitate the movement of keratinocytes from the epidermis.6 Algorithms of care are predicated upon the underlying wound etiology. Dead space is often managed with packing, drains, antibiotic beads and/or NPWT. Offloading remains a critical element in the treatment algorithm when addressing neuropathic ulcers in patients with diabetes. Evidence supports the use of total contact casting or instant total contact designs as the most effective and cost-efficient methodology once infection is controlled; however, pressure relief must be individualized to the patient and evaluated at each encounter.
CASE REPORT
This 58 year-old white male with insulin dependent diabetes presented with a fulminant infection of the left foot. Symptoms started 3 days prior, subsequent to wearing a tight shoe. (Fig 3) The foot was painful despite diabetic neuropathy. A recent distal bypass surgery appeared patent. The patient was admitted to the hospital for emergent medical and surgical treatment. He had a temperature of 101° F accompanied by chills. Blood work confirmed leukocytosis consistent with a serious infection. X-ray revealed gas in the soft tissue. A diagnosis of deep space infection and sepsis was formulated and the patient was taken urgently to the operating room for intervention. A multidisciplinary team consisting of vascular, podiatry, infectious disease, and internal medicine was convened.
 Figure 3. Fulminant infection with sepsis
Figure 3. Fulminant infection with sepsis
An open amputation was performed (Fig 4) and NPWT with instillation was instituted. Bone biopsy was negative for osteomyelitis. The patient was subsequently discharged with intravenous antibiotics and NPWT. The patient was followed weekly for debridement and surveillance. Offloading was accomplished with a CAM Walker. Home healthcare was instituted for 4 weeks and NPWT was discontinued after 2 weeks in favor of collagen-ORC with silver. After 3 weeks, the dressing was changed to collagen-ORC until closure.
Unfortunately, due in large part to non-adherence, the patient subsequently presented with another significant infection in the same foot requiring re-admission. His temperature on admission was now 99.1° F and his white count was normal. X-rays and MRI were negative for gas and osteomyelitis. (Fig 5)
 Figure 5. Poor adherence lead to re-infection
Figure 5. Poor adherence lead to re-infection
An aggressive debridement was performed, and the wounds were covered with cadaveric allograft. (Fig 6 & 7) NPWT with instillation was instituted, and the patient was again discharged with NPWT and intravenous antibiotics. The case manager was meticulous about coordinating his care, including home health, care of PICC line and antibiotics, hyperbaric oxygen and wound care appointments. Three weeks later he was readmitted for a split thickness skin graft (Fig 8) and went on to heal uneventfully.
 Figure 6. Extensive debridement
Figure 6. Extensive debridement
CONCLUSION
Patients with diabetes frequently develop serious infections requiring hospitalization. After appropriate therapy, the patient must be transitioned to the outpatient environment with meticulous attention to detail. Absent this important step, the patient may be lost to follow-up and suffer serious consequences. However, as this case clearly elucidates, lack of patient concordance often leads to recidivism.
 Figure 7. Application of cadaveric allograft
Figure 7. Application of cadaveric allograft
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
References
1.Lavery LA, Armstrong DG, Murdoch DP, Peters EJG, Lipsky BA. Validation of the Infectious Disease Society of America’s diabetic foot infection classification system. Clinical Infectious Diseases. 2007; 44: 562-5
2. Moore Z, Butcher G, Corbett L, Snyder R, McGuiness W, van Acker K. AAWC, AWMA, EWMA Position Paper: Managing Wounds as a Team. J Wound Care. 2014; 23(5 Suppl.): S1-S38
3.Mitchell P, Wynia M, Golden R, McNellis B, Okun S, Webb CE, Rohrbach V, Von Kohorn I. Core principles & values of effective team-based health care. Discussion Paper, Institute of Medicine. Washington, DC. 2012. www.iom.edu/tbc Accessed 24 April 2016
4.Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJG, et al. 2012 Infectious Disease Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clinical Infectious Diseases. 2012; 54(12): 132-173
5.Woo K, Krasner D, Kennedy B, Wardle D; Moir O. Palliative wound management strategies for palliative patients and their circles of care. Advances in Skin & Wound Care. 2015; 28(3): 130-140
6.Snyder RJ, Fife C, Moore Z. Components and quality measures of DIME (devitalized tissue, infection/inflammation, moisture balance, and edge preparation) in wound care. Adv Skin Wound Care. 2016; 29; 205-215
7.Snyder RJ, Frykberg RG, Rogers LC, Applewhite AJ, Bell D, Bohn G, Fife CE, Jensen J, Wilcox J. The management of diabetic foot ulcers through optimal offloading. J Am Podiatr Med Assoc. 2014; 104(6): 555-567



