Dr. Orgill is Vice Chairman for Quality Improvement in the Department of Surgery at Brigham and Women’s Hospital and Professor of Surgery at Harvard Medical School. He is a reconstructive plastic surgeon and has a PhD from MIT in Medical Engineering. He is the Director of the Brigham and Women’s Hospital Wound Care Center and runs a tissue engineering and wound healing Laboratory. His lab at BWH is working to develop better technologies to treat wounds including work with artificial skin, micromechanical forces, platelets and stem cells. He has consulted for several medical device and start-up companies and is the inventor on several patents. He worked on the team that developed Integra®, a skin replacement therapy that has been commercially developed and used successfully on thousands of patients.
Orgill_Current Dialogues in Wound Management_2015_Volume 1_Issue 4
Complex bone and soft tissue defects present the surgeon with myriad potential reconstructive approaches. The reconstructive ladder, a classic plastic surgery teaching, assists the surgeon in selecting an option, by suggesting the easiest approach that will satisfy the demands of the patient. The reconstructive ladder has been heavily critiqued over the years because it does not take into account the following two important considerations:
1)Sometimes the best method to reconstruct a defect may be the most complex method on the ladder. For example, in breast reconstruction, the easiest method would be simple closure of the mastectomy flaps, yet many surgeons do complex implant-based fat grafting or construct perforator flaps, which are really not part of the ladder.
2)Use of new technologies, such as negative pressure wound therapy, cell-based therapies, and soft tissue scaffolds can very often allow the surgeon to use a simpler rung of the reconstructive ladder.
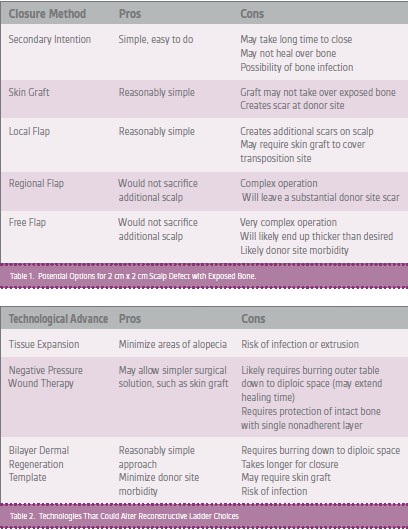
A hypothetical reconstructive case can illustrate use of the reconstructive ladder: a 47-year-old female has sustained a scalp injury, which leaves a 2.0 cm x 2.0 cm defect with exposed bone. How should the surgeon attempt to close this defect? The surgeon would review the various options on each rung of the ladder, listing the pros and cons of each approach (Table 1), and, in consultation with the patient, determine and implement the decision that made the most sense.
The surgeon could also consider new technologies and options outside the reconstructive ladder (Table 2). Although these technologies lengthen the time to definitive closure of the wound, they have the potential to improve the donor site, simplify the reconstructive approach, or achieve a better functional result.
The expertise of the surgeon and the setting of care delivery also influence selection of the reconstructive method. Advanced technologies may not be available in all hospitals. In this situation, the reconstructive ladder provides an outstanding paradigm. In addition, a skilled surgeon with expertise in microsurgery or complex procedures, such as tissue expansion, may not be readily available in all settings. Even when these providers are available, wide variation in their experience guides selection of a surgeon for a specific patient. For example, some centers in the United States have considerable experience with either implant- or perforator flap-based breast reconstruction. Therefore, a woman’s selection of a surgery center strongly influences the type of reconstruction she is likely to receive.
Clearly, more data are needed to help medical practitioners and surgeons determine the optimal procedure or technology for a given patient. Prospective randomized clinical trials have been considered the gold standard to assist in making these difficult decisions, but they are difficult to perform to assess complex surgical procedures, due to the variation in surgical technique. Often, trials do not accurately reflect clinical practice as they exclude many patients who require treatment. Registry-based data collection systems may offer better real-life information to help guide selection of surgical procedures and technologies and may facilitate generation of data on the cost and value of different procedures.
In summary, the reconstructive ladder is a useful paradigm to help surgeons work through a variety of options for patients requiring reconstruction. Modifications to this ladder to include new technologies and the capacity of specific care settings could also be quite useful.
References
Erba P, Ogawa R, Vyas R, Orgill DP. The reconstructive matrix: a new paradigm in reconstructive plastic surgery. Plast Reconstr Surg. 2010;126(2):492-8.