
Emily Greenstein, APRN, CNP, CWON, FACCWS is a Certified Nurse Practitioner at Sanford Health in Fargo, ND. She is certified as an Adult-Gerontology Nurse Practitioner through the American Academy of Nurse Practitioners. She has been certified in wound and ostomy care through the WOCNCB for the past 9 years. At Sanford she oversees the outpatient wound care program, serves as chair for the SVAT committee and is involved in many different research projects. Ms. Greenstein is a paid consultant for 3M.
Greenstein_Current-Dialogues-in-Wound-Management_2021_Article-13
Venous ulcers are the most common ulcer of the lower limb and often have increased exudate due to chronic venous hypertension that can cause the vein walls to leak fluid and proteins.1,2 Excessive wound exudate can result in pooling at the wound bed and can cause maceration of the wound surface, resulting in cells that are overhydrated and vulnerable to minor trauma as well as an increased risk for the development of hypergranulation tissue.3 Additionally, maceration of the periwound skin can also result, leading to the potential for periwound skin breakdown, wound enlargement, increased risk for infection, further impaired healing, and pain. Strategies to manage highly exudative venous leg ulcers (VLUs) include, periwound skin protection, appropriate primary and secondary dressing selection, and the use of correct compression therapy.
PERIWOUND ASSESSMENT
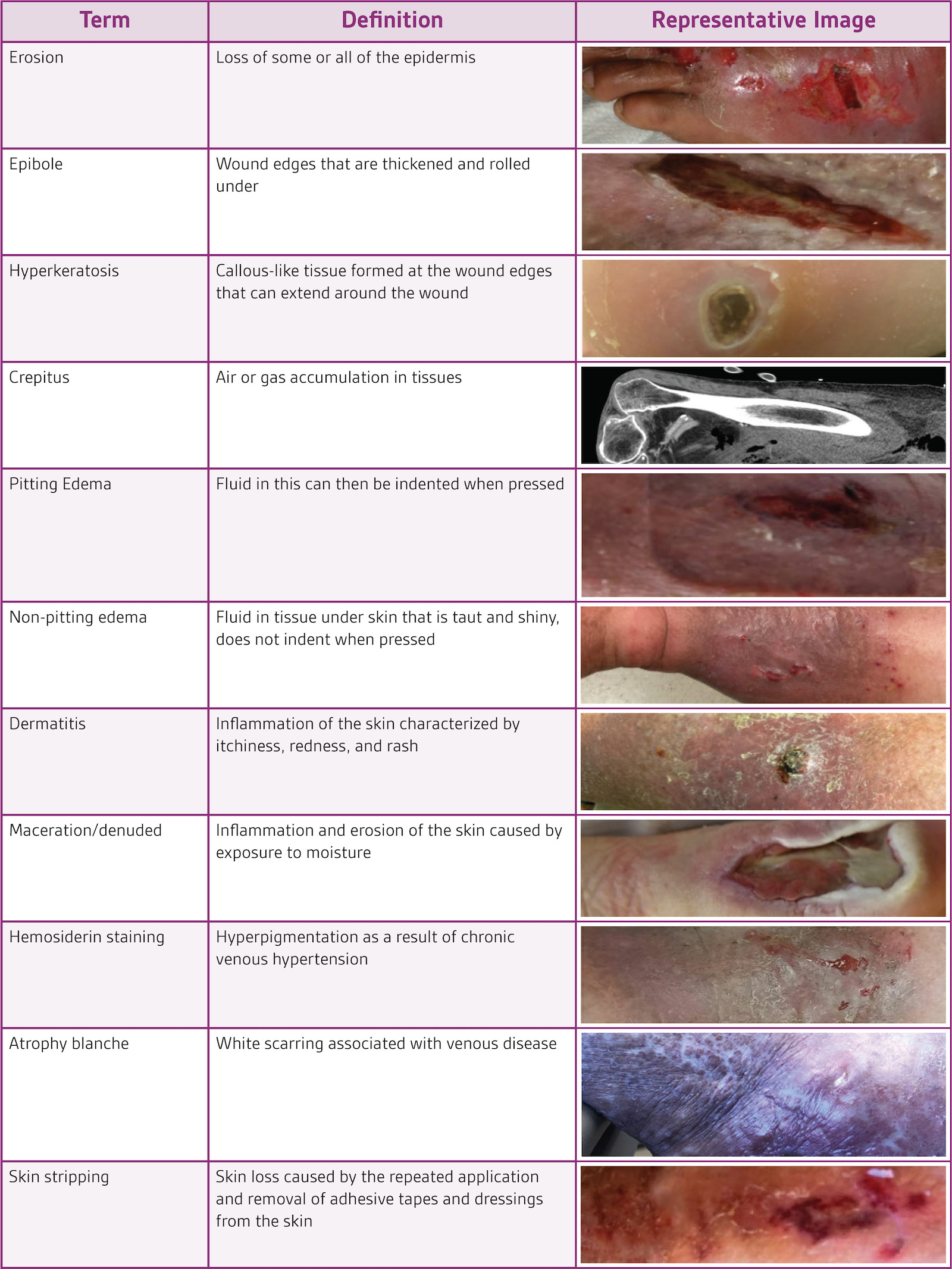
A major component to the healthcare provider’s VLU treatment plan is the periwound skin assessment. The assessment should include the periwound and surrounding skin, extending 4 cm from the wound bed. When performing the assessment, key factors to keep in mind are skin temperature, wound location, periwound shape, periwound color, and exudate amount. Common terms associated with periwound skin conditions are listed in Table 1.
MANAGEMENT OF MACERATION
With the condition of the periwound skin identified, a plan to prevent, treat, and manage periwound skin to ensure wound healing progress should be created. The clinician should select wound and skin care products based on the wound and periwound skin status with frequent reassessments allowing for treatment plan modifications as necessary.
For maceration, treatment principles focus on reducing excessive moisture. There are several ways of preventing exudate-related damage to the extracellular matrix and periwound skin. The first way to avoid damage to the periwound skin is to prevent wound exudate from coming into contact with it through the use of specialty dressings. The ideal primary and secondary dressings are those that conform to the wound surface, prevent dead space, and absorb a large amount of exudate with the goal of wicking exudate away from the wound surface and preventing maceration. One product example that can be used is 3M™ Kerramax Care™ Super-Absorbent Dressing (Figure 1). This dressing has a wicking layer that evenly distributes fluid both horizontally and vertically throughout the dressing, utilizing the full absorption capacity.

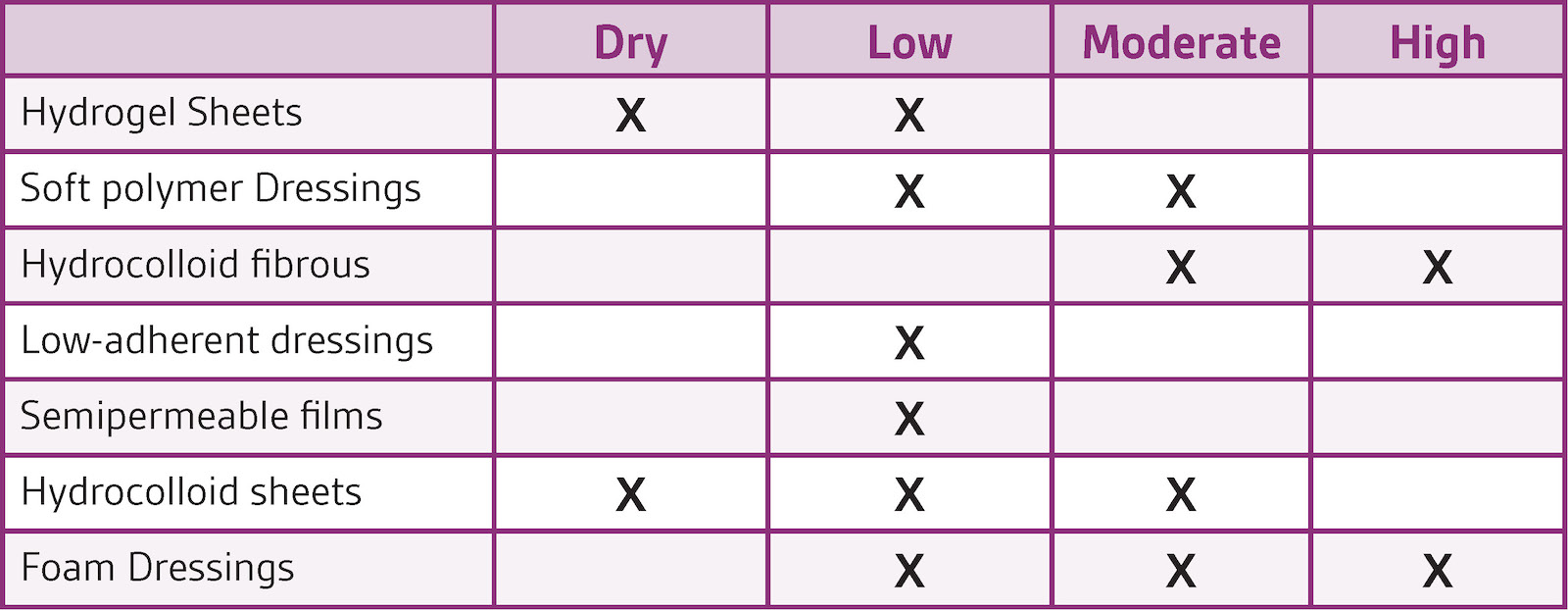
A wide range of absorptive dressings are available, and care should be taken to match the dressing’s absorptive qualities to the amount of exudate present with frequent reassessments as exudate levels change as the wound heals
(Table 2). Common consequences of improper exudate management are periwound maceration or desiccation, which can be the result of mismatch between absorptive capacity of the dressing, frequency of dressing changes, or both. If maceration is severe enough, it will damage the existing epithelium to the point that healing is slowed or stopped. On the other hand, desiccation occurs from insufficient moisture.3 Dressings with high absorptive capacity may promote periwound dryness if exudate is not appropriately assessed and further changes made to the dressing combinations or frequency of changes.
USE OF PROTECTIVE SKIN AGENTS
The use of protective skin agents can be beneficial for patients with VLUs and can help prevent periwound skin damage. The area needing protection, the amount of drainage, and the frequency of dressing changes should be taken into account during skin protectant product selection. Protective skin agents are available in ointments, sprays, creams, wipes, wand applications, and more. Common preparations include petroleum, zinc, silicone/dimethicone, polymer films, and cyanoacrylates. These products are easy to apply and can protect skin from dressing-related trauma. Clinicians should always refer to the manufacturer’s instructions for use when selecting and applying the dressings. Using a skin protectant (liquid or spray) on the periwound and surrounding skin can help to lessen friction forces. Use of zinc barrier creams for VLU periwound skin can be difficult due to unwanted product buildup during application and/or epidermal stripping upon removal. Skin protectant alternatives to barrier creams include 3M™ Cavilon™ No Sting Barrier Film and 3M™ Cavilon™ Advanced Skin Protectant.
Cavilon No Sting Barrier Film is a terpolymer based alcohol-free barrier film that provides protection from skin damage. It is flexible and conforms to the skin during movement and position changes allowing for a continuous skin protection barrier. Cavilon Advanced Skin Protectant is a revolutionary polymer-cyanoacrylate technology that is designed to manage moderate to severe skin damage and protect at-risk skin. It attaches well to wet, weepy, damaged skin and can last up to 7 days.
In conclusion, VLUs can be highly exudative wounds, resulting in an increased risk for periwound skin breakdown. Periwound skin damage can exacerbate pain, increase wound size and delay healing, thereby increasing healthcare costs and reducing patients’ quality of life.3 As such, periwound skin should be regularly assessed and the appropriate dressing and skin protectant products should be selected to help prevent damage and manage the periwound skin condition as early as possible during VLU care.
References
References:
1. Nussbaum SR, Carter MJ, Fife CE, et al. An Economic Evaluation of the Impact, Cost, and Medicare Policy Implications of Chronic Nonhealing Wounds. Value Health. 2018;21(1):27-32.
2. Sumpio BE, Blume P, Mena-Hurtado C. Lower Extremity Ulceration. In: Creager M, Beckman J, Loscalzo J, eds. Vascular Medicine: A Companion to Braunwald’s Heart Disease. 3rd ed. Philadelphia, PA: Elsevier; 2020:836-848.
3. Cutting KF. Wound exudate: composition and functions. Br J Community Nurs. 2003;8(9 Suppl):4-9.
4. Tate S, Price A, Harding K. Dressings for venous leg ulcers. British Medical Journal. 2018;361:k1604.
NOTE: Specific indications, contraindications, warnings, precautions, and safety information exist for these products and therapies, some of which may be Rx only. Please consult a clinician and product instructions for use prior to application.
© 2022 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. 3M Marks used under license in Canada.

