
Dr. Jonathan Arnold obtained his medical degree in 1997 from the University of Oklahoma College of Medicine in Oklahoma City.
He is board certified by the American Board of Family Medicine, the American Board of Preventive Medicine – Undersea and Hyperbaric Medicine (ABPM-UHM). He is also credentialed by the American Board of Wound Management as a Certified Wound Specialist Physician (CWS-P)
Arnold_Current-Dialogues-in-Wound-Management_2019_Article_4
Since its inception, negative pressure wound therapy (NPWT) has been used to promote granulation tissue development and remove infectious materials. Medical advancements have also led to the evolution of standard NPWT to new iterations, including mechanically powered NPWT and an increased selection of device-associated dressings. This improved selection of NPWT options allows for the NPWT system to be matched to the patient and wound.
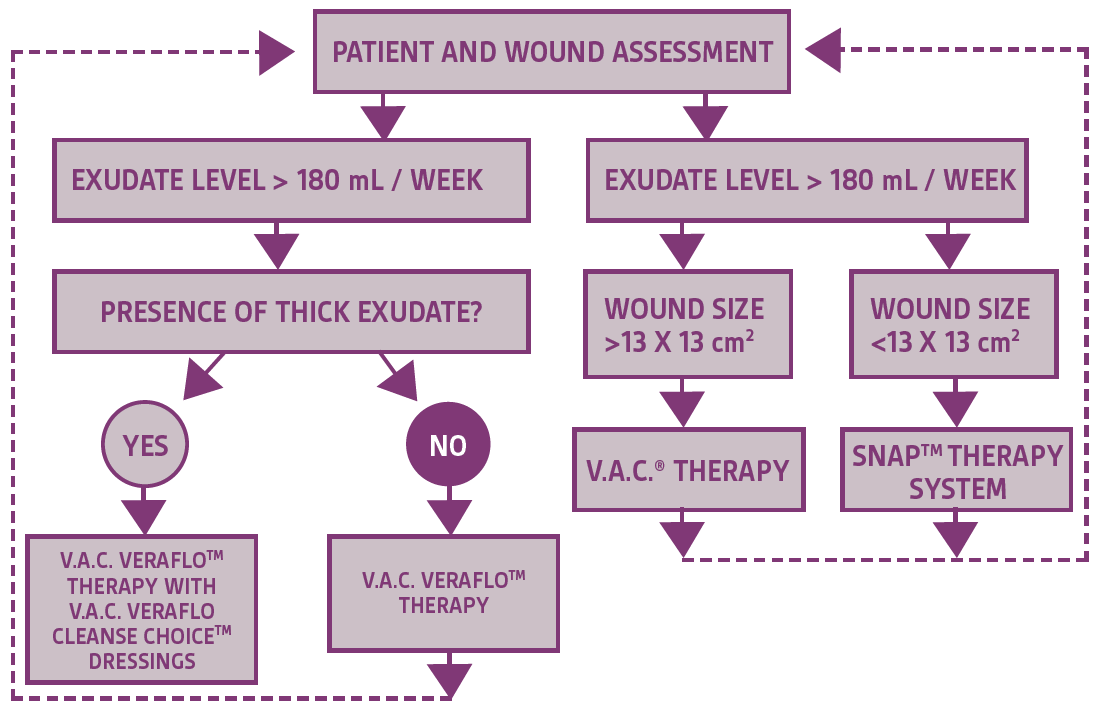
Despite the plethora of NPWT options, it can be difficult for the health care provider to determine when it is appropriate to transition patients from one NPWT system to another. In my practice, NPWT system selection is based on wound characteristics such as the amount of exudate, presence of thick exudate, and wound size (Figure 1). Additional factors that I consider for treatment selection include device weight, device noise level, need for electricity, and ability to conceal the device.
REPRESENTATIVE CASES
Case 1
A 60-year-old male with a history of morbid obesity, hypertension, and impaired glucose tolerance was referred to the outpatient wound clinic three weeks after wound dehiscence following extensive ventral hernia repair (Figure 2).

The wound was cleansed in the operating room, and wound cultures were obtained. Initial wound management utilized wet-to-dry dressings. Oral antibiotics were started when the wound cultures were positive for Pan-sensitive Staphylococcus aureus. Traditional V.A.C.® Therapy was then initiated with dressing changes every 2-3 days and continued while the wound showed signs of depth reduction and development of granulation tissue (Figure 3).

Once the wound drainage was reduced to <180 mL/week, therapy was switched to mechanical NPWT using the SNAP™ Therapy System. The wound continued to show improvements (Figure 4) and was fully closed following 21 days of SNAP™ System use (Figure 5).


For this patient, continued use of the SNAP™ System was ideal due to reduced amount of drainage and desire of the patient to maintain mobility and conceal the device.
Case 2
A 69-year-old female presented to the emergency department with blistering of the left lower extremity and progressive pain over 2 months. Previous medical history included obesity, diabetes, diabetic neuropathy, and coronary artery disease. Initial treatment included failed revascularization surgery and subsequent below-the-knee amputation (BKA). The incision dehisced 10 weeks after surgery. A wound infection developed and was treated with topical and intravenous antibiotics. Oral antibiotics were also used following patient discharge. However, the wound continued to worsen, and the BKA site was injured following a direct impact fall. Increasing drainage, pain, and fever developed subsequent to the fall, and the patient was readmitted to the hospital. Surgical debridement was performed followed by application of V.A.C.® Therapy (Figure 6). Dressing changes occurred every 2-3 days. An above-the-knee amputation for revision was recommended but was declined. The patient received broad-spectrum intravenous antibiotic coverage following a consult with the infectious disease department. After 29 days of V.A.C.® Therapy, human acellular dermis was applied over deeper wound areas followed by use of a non-adherent cover layer and V.A.C.® Therapy as a bolster with dressing changes every 2-3 days (Figure 7).


The wound showed development of granulation tissue 4 weeks after the graft was applied (Figure 8). After 9 weeks, treatment was transitioned to mechanical NPWT using the SNAP™ System as the wound showed reduction in drainage and size (Figure 9). After 39 days of SNAP™ System use wound reduction was noted (Figure 10). Wound care was switched to topical collagenase and topical antibiotic ointment after 11 weeks of SNAP™ System use (Figure 11).




CONCLUSION
Since the inception of NPWT, therapeutic evolutions have allowed health care providers to optimize device and dressing selection to the patient and the wound. However, as wound healing progresses, treatment requirements change. It is important for the healthcare provider to continually assess the patient and wound and adjust the treatment plan as necessary.1 One such adjustment is customizing the NPWT system used to the wound and knowing when to discontinue NPWT use altogether. Continual assessment of the patient’s needs and wound characteristics can help the clinician when selecting initial NPWT system use as well as when wound care should be transitioned from traditional NPWT to mechanical NPWT. Wound healing can be a difficult process as shown; however, by examining the wound characteristics, the wound treatment plan can be adjusted to suit the needs of the wound and the patient.
References
- Gupta S, Andersen C, Black J et al. Management of Chronic Wounds: Diagnosis, Preparation, Treatment, and Follow-up. Wounds 2017;29(9):S19-S36.
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
Specific indications, contraindications, warnings, precautions and safety information exist for KCI products and therapies. Please consult a clinician and production instructions for use prior to applications. This material is intended for healthcare professionals.

