Rose Raizman’s nursing career spans more than 20 years in a variety of nursing positions. Currently she is applying her passion for helping people to obtain and maintain optimal level of health as a wound care NP at community hospital in Ontario, Canada. Rose received Master of Medicine from Hebrew University in 2001 in Israel and Master of Nursing combined with Primary Health Nurse Practitionner in 2015 in Canada. She holds CNA certification in Enterostomal Therapy and her primary areas of expertise are ostomy, wound and continence care in all care settings. She has presented and published her work nationally and internationally.
Raizman_Advanced Wound Dressings Today_Advanced Wound Dressings Today_2017_Spring Supplement
Currently the most accepted paradigm of successful wound care is “DIME” or “TIME”1 where clinicians are called upon to first address tissue viability and debride devitalized tissues from the wound (D or T in the acronym), eliminate infection (I), address moisture (M) balance in the wound, and promote epithelial growth by ensuring that edges (E) of the wound are contracting. Striving for cost efficiency and optimal patient outcomes, clinicians often try to find a therapy that would address all domains simultaneously. Unfortunately, only one modality cannot, often times, address all these needs, thus a combination of therapies is required. For example, the wound bed would be cleansed by an appropriate solution, followed by debridement, and a suitable wound cover dressing, or combination of such dressings chosen.
To help clinicians in this important and challenging task, the wound care industry is developing dressings and technologies. However, the fast pace of these innovations has become a challenge for wound care clinicians in terms of staying current and being aware of interactions between therapies or dressings that could potentially deactivate one another. Antiseptic preparations are those that non-selectively reduce flora on the surface of the skin or wound bed. Some have been found to be cytotoxic to fibroblast keratinocytes and leukocytes in vitro, but in vivo no such correlation has been confirmed and they have been rendered to be safe, yet controversies about their usage still exist.2, 3 In depth chemical analysis or effectiveness of these therapies and cleansers is beyond the scope of this paper.
This paper reviews the role of cleansing solutions in wound care and some possible interactions leading towards inactivation of key components of advanced wound dressings. The most common choice of cleansers include: sodium chloride, water, iodine, chlorhexidine, hypochlorous acid-based cleansers and commercially available cleansers that contain surfactants. The active ingredients within dressing components are varied and numerous but common elements are silver, iodine, polyhexamethylene biguanide (PHMB), gentian violet/methylene blue, and pDADMAC. The predominant concern from a clinical perspective is that the components within the cleanser and the active wound dressing ingredient could deactivate one another’s clinical benefits and detract from the healing process.
Let’s review the possible interactions among the antiseptic solutions and wound dressings with active ingredients:
BIGUANIDES
CHLORHEXIDINE GLUCONATE was formulated from a series of bisbiguanides processing which has a marked bacteriocidal action against a wide range of microorganisms.4 Chlorhexidine gluconate is believed to have anti-inflammatory effects on the tissue. Lower concentrations (e.g. 0.02%) are recommended for use in wound irrigation.5 Its possible mode of action is combining with the cell surface, disorganizing permeability barriers and coagulating the cytoplasmic content of the cells.
Activity of chlorhexidine is pH dependent and is reduced in the presence of organic matter, blood or pus.7 Chlorhexidine is believed to be fairly compatible with most available dressings, although caution should be employed when combining silver nitrate and chlorhexidine preparations. Even a 0.5% of silver nitrate when combined with 0.02% chlorhexidine gluconate solution leads to precipitation of chlorhexidine nitrate.
Another possible interaction leading to perchloric acid (PCA) precipitate is with hypochlorous acid. An immediate reaction can be observed when 2.0% chlorhexidine (CHX) is combined with sodium hypochlorite (NaOCl), even at a low concentration (0.023%). Therefore, these should not be combined or used unless washed out with a neutral solution.
POLYHEXAMETHYLENE BIGUANIDE (PHMB) is a small cationic polymer that is used as an antiseptic and in a variety of advanced wound care products as it appears to be highly histocompatible and non-cytotoxic.4 It transfers from the surface of the bacteria to the cytoplasm, especially when pH is between 5-6, and leads to bacterial death due to release of lipopolysaccharides and potassium ion efflux.10
PHMB (as in Kerlix™ AMD, Covidien LP, Mansfield, MA) deactivates sodium hypochlorite and enzymatic debriders.1 In contrast, pDADMAC (e.g. Bioguard®Dressings, Quick-Med Technologies, Inc., Gainsville, FL) are large cationic polymers that are safe with enzymatic debriders (e.g. Santyl® Oinment, Smith & Nephew, Inc., Memphis, TN).
POVIDONE IODINE (PVP-I) is a chemical complex composed of molecular iodine and polyvinylpyrrolidone (povidone), commonly used for wound irrigation. Povidone iodine has been Food and Drug Administration (FDA) approved for the short-term treatment of superficial and acute wounds.12 Iodine impregnated dressings as well as cadexomer iodine are commonly used topical treatments. Note that iodine is contraindicated in patients with thyroid disease after treatment with radioiodine, patients with Duhring disease, iodine allergy sensitivity, perturbation of neonatal thyroid hormone, and when extensive body areas are exposed due to risks of systemic toxicity.13 Some authors suggest that slow replacement of neutral lipids in elderly can increase exposure to iodine from povidone iodine in the elderly.14 Iodine reacts with hydrogen peroxide, silver, taurolidine (used for catheter related bloodstream infections), mercury, and proteins, rendering them ineffective.6,15
HYPOCHLOROUS ACID (HOCL) is highly active against all bacterial, viral, and fungal human pathogens and can kill spore-forming and non-spore bacteria in a relatively short period of time. Its intended use is for cleansing (or deep cleaning), irrigating, and debriding acute and chronic wounds.2 Hypochlorous acid leads to cell death by the oxidation of sulfhydryl enzymes and amino acids, ring chlorination of amino acids, loss of intracellular contents, decreased uptake of nutrients, and inhibition of protein synthesis, decreased oxygen uptake, oxidation of respiratory components, decreased adenosine triphosphate production, breaks in DNA, and depressed DNA synthesis.16
The original Dakin’s solution (pH 9 to 10) is known to be cytotoxic to healthy cells and granulating tissue, and as such its use is not recommended for periods longer than 7-10 days16 and limited to use in wounds requiring extensive debridement. However, recently HOCL solution has regained popularity and new manufacturing processes have allowed for a change in pH ranges (3.5-5.5 etc), oxidation-reduction potential (ORP), HOCL concentrations and thus the overall safety profile of these cleansers has improved.17
SILVER is widely used as an active component in a vast variety of dressings (e.g. cleansers, alginates, gels/ointments, foams, collagen, and ORC/collagen preparations). Silver ions are believed to act by binding to the DNA helix and blocking transcription.4While some companies explicitly recommend the use of Sterile Water to cleanse the wound to prevent interaction between Sodium and Argentum Ions, others leave it up to the clinicians to choose.
It is important to note that bodily fluids have a physiologic concentration of sodium and thus some neutralization will happen regardless of an irrigation solution. However, unbound iodine molecules can neutralize Silver Ions more readily and therefore clinicians should refrain from combining Silver and Iodine based products. If Iodine irrigation is still required, rinsing the wound afterwards with a neutral solution such as water or saline is recommended.
Both Silver and Iodine inactivate growth factor therapies and are also advised not to be used with enzymatic debridement.1,11
GENTIAN VIOLET AND METHYLENE BLUE (GV/MB) antibacterial dressings consisting of organic antimicrobial dyes have been used for many years in the clinical setting with minimal toxicity to humans. Both GV and MB dyes are basic with a positive charge, thus showing differential activity toward gram-negative versus gram-positive bacteria.18 Gentian Violet and Methylene Blue are contraindicated in 3rd degree burns.19 No specific stated interactions of these dressings with other agents available on the market are reported in the literature or noted by manufacturers in their product monographs or package inserts.
Let’s look at a few examples:
CASE 1
A 74 year-old male presented with an infected diabetic wound ulcer on the left foot. During baseline assessment, the wound measured 6 cm x 7 cm x 3 cm and was 100% covered with slough. A probable bone involvement was suspected. The standard care for a person with diabetes who has developed a wound should involve a multidisciplinary team approach (infectious disease, surgeon, chiropodist or podiatrist, dietitian, endocrinologist, etc.) along with initial sharp debridement and initiation of systemic antibiotics. The wound care regimen prescribed consisted of using negative pressure (V.A.C. VERAFLO™ Dressing Kit – Medium 2 foam dressings [17 x 15 x 1.8cm]) with one quarter Dakins solution (Negative Pressure Wound Therapy with instillation and dwell time (NPWTi-d) (V.A.C. VERAFLO™ Therapy, KCI, San Antonio, TX). At this stage reducing bioburden while removing necrotic tissue was of great importance. Since the wound was completely covered by slough, there were no concerns of cytotoxicity when an irrigation solution was chosen. It should also be noted that systemic absorption was highly improbable at that point. Quarter strength Dakins solution was chosen in this particular case. It is very important to remember that hypochlorous acid, chlorhexidine and PHMB should not be used together in any combination to prevent deactivation of active components.
The following week, the wound had 80% of granulation tissue growth with exposed bone—which was assumed to be osteomyelitis but was not confirmed by x-ray— and moderate exudate. A change in the wound care regimen needed to be established to address bioburden, possible cytotoxicity, and moisture control. Peer-reviewed literature using an in vivo model supports the approach to cleanse the wound with povidone iodine or chlorhexidine. However, caution should be exercised that silver dressings should not be used concomitantly with an iodine-based cleanser due to possible interactions. Therefore, if a decision is made to apply a silver-based foam or ORC Collagen with silver, the wound care choice should be a chlorhexidine-based cleanser.
At follow up appointments, the wound progressed towards proliferation and epithelialization and thus the subsequent cleansers of choice were saline or tap water.20 Although both solutions are non-cytotoxic and can be used as wound irrigation solutions, one should always keep in mind that saline preparation should not be left open for longer than 24 hours to prevent contamination.
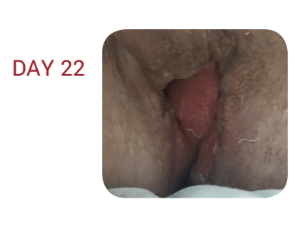
CASE 2
A 69-year-old male presented with perineal Fournier’s Gangrene and an abdominal abscess. The patient was started on intravenous antibiotics.
The wound had 100% necrotic tissue so the goals of therapy were wound bed preparation by removal of necrotic tissue and infectious materials and granulation tissue formation. The cleanser of choice at this stage should address the opportunity to apply a continuous cleansing solution for ongoing irrigation. Current research shows no clear advantage of any particular irrigation solution.21, 22 The choice for this wound was Negative Pressure Wound Therapy with instillation and dwell time (NPWTi-d) (V.A.C. VERAFLO™ Therapy, KCI, San Antonio, TX) with Hypochlorous Acid 1:20. NPWTi-d settings included a 10 minute dwell time and 4 hours of continuous negative pressure at -125 mmHg. Dressings were changed 3 times per week.
The wound presented with mixed necrotic and granulation tissue. Conservative sharp wound debridement involving the removal of necrotic and devitalized tissue at the bedside with scissors was commenced. The goals remained the same (removal of necrotic tissue and infectious materials as well as granulation tissue formation). Dressing changes were conducted as per protocol and were changed 3 times per week.
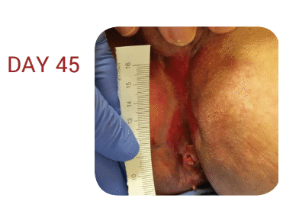
The wound reached 100% granulation with moderate discharge and a wound depth of 1 cm.
The main goals at this point were to address an edge effect and maintain moisture control. Therefore NPWTi-d was discontinued; however, we continued the use of NPWT without irrigation to promote further granulation tissue, ensure exudate was managed (to promote moisture control and create the optimal healing environment). Supportive cleanser to manage bioburden was Povidone –iodine Solution.
The wound bed reached 100% granulation with minimal discharge. The edges were level with the wound bed and NPWT was discontinued.
As the edge effect and moisture control were the final goals, one more challenge still existed insofar as the wound had a close proximity to the anus. Antimicrobial control was also a consideration to enhance optimal healing at this final stage.
A supportive cleanser of choice should be non-cytotoxic and compatible with the dressing that has been selected. In order to maintain the edge effect, the dressing of choice can be a collagen or silver based collagen.
The cleanser that was chosen in this particular case was chlorhexidine 2%. ORC Collagen with silver was applied as a topical treatment, and a foam dressing was used to maintain moisture balance and changed every 2-3 days. It should be noted that Povidone Iodine was discontinued due to possible interactions with silver dressings.
The wound was close to being fully epithelialized. At this stage, moisture balance and edge effect were most important. The supportive cleanser was non-toxic (such as NaCl 0.9% or tap water) and an absorptive dressing such as self-adherent foam for less frequent dressing changes (2-3 days) or a gauze dressing if dressing changes are frequent (e.g. after each bowel movement or a trip to the washroom) may be used. In this particular case foam was chosen as per patient preference.
CONCLUSION
Wound care practitioners should engage in comprehensive approaches that involve both patients and multidisciplinary team members. Both ‘art and science’ are required while deciding on optimal care plans. Clinicians should remember that the composition of dressings and cleansers can contain either ionic or salt components of the metals and therefore there are potential chemical interactions that can deactivate active components.
It should be remembered that metal ions can interact with each other or other substrates. For example, refrain from combining silver based dressings with iodine based dressings. In addition, manufacturer’s instructions should be consulted for the choice of preferred cleansing agents.
References
1. Cowan, Linda, et al. Caution: when combining topical wound treatments, more is not always better. Wound Practice & Research: Journal of the Australian Wound Management Association 19.2 (2011): 60.
2. Armstrong D, Bates-Jensen B, Bohn G, et al. Expert recommendations for the use of hypochlorous solution: science and clinical application. Wounds. 2015.
3. Scanlon, E., and Stubbs, N. To use or not to use? The debate on the use of antiseptics in wound care. British journal of community nusring 7. Sup2 (2002): 8-20.
4. Atiyeh, B. S., Dibo, S. A., & Hayek, S. N. (2009). Wound cleansing, topical antiseptics and wound cleansing, topical antiseptics and wound healing. International Wound Journal, 6(6), 420-430.
5. Drosou A, Falabella A, Kirsner RS. Antiseptics on Wounds: An Area of Controversy. Wounds. 2003; 15(5):149-166.
6. Mulder GD, Cavorsi JP, Lee DK. Antimicrobial Agents in Wound Care. Wounds. 2007;19(7):173-182.
7. McDonnell G, Russell AD. Antiseptics and disinfectants: activity, action, and resistance. Clin Microbiol Rev.1999; 12(1):147-179.
8. Senior N. Some observations on the formulation and properties of chlorhexidine. J Soc Cosmet Chem. 24(4): 259-278.
9. Basrani BR, Manek S, Sodhi R, Fillery E, Manzur A. Interaction between sodium hypochlorite and chlorhexidine gluconate. J Endod. 2007; 33(8): 966-969.
10. Yasuda K, Ohmizo C, Katsu T. Potassium and tetraphenylphosphonium ion-selective electrodes for monitoring changes in the permeability of bacterial outer and cytoplasmic membranes. J Microbiol Methods. 2003;54(1):111-115.
11. Jovanovic A, Ermis R, Mewaldt RS, Shi L, Carson D. The Influence of Metal Salts, Surfactants, and Wound Care Products on Enzymatic Activity of Collagenase, the Wound Debriding Enzyme. Wounds. 24(9):242–253.
12. Safety and effectiveness of consumer antiseptics; topical antimicrobial drug products for over-the-counter human use; proposed amendment of the tentative final monograph; reopening of administrative record; proposed rule. Fed Regist 78:76444–76478. http://www.gpo.gov/fdsys/pkg/FR-2013-12-17/pdf/2013-29814.pdf
13. Khan M, Naqvi AH. Antiseptics, iodine, povidone iodine and traumatic wound cleansing. J Tissue Viability. 2006; 16(4):6-10.
14. Smith RG. Critical discussion of the use of antiseptics in acute traumatic wounds. J Am Podiatr Med Assoc. 2005; 95(2):148-153.
15. Schmitz G. Iodine oxidation by hydrogen peroxide and Bray–Liebhafsky oscillating reaction: effect of the temperature. Phys Chem Chem Phys. 13(15): 2011: 7102-7111. doi: 10.1039/C1CP00006C
16. Sakarya S, Gunay N, Karakulak M, Ozturk B, Ertugrul B. Hypochlorous Acid: an ideal wound care agent with powerful microbicidal, antibiofilm, and wound healing potency. Wounds. 2014; 26(12):342-350.
17. Thorn RM, Lee SW, Robinson GM, Greenman J, Reynolds DM. Electrochemically activated solutions: evidence for antimicrobial efficacy and applications in healthcare environments. Eur J Clin Microbiol Infect Dis. 2014; 31(5):641–653.
18. Edwards K. New Twist on an Old Favorite: Gentian Violet and Methylene Blue Antibacterial Foams. Adv Wound Care(New Rochelle). 2016; 5(1): 11–18.
19. Hydrofera Blue Classic Antibacterial Foam Dressing; SDS HB2214/HB4414-00 Safety [Online]; Hollister: Libertyville, IL, April 13, 2016. http://www.hollister.com/~/media/files/pdfs%E2%80%93for%E2%80%93download/sds/sds%E2%80%93hydrofera%E2%80%93blue%E2%80%93classic.pdf?la=en (accessed April 15, 2017)
20. Chao C, Runde D. Tap Water vs. Sterile Saline for Wound Irrigation. Am Fam Physician. 2015; 92(3). http://www.thennt.com/nnt/tap-water-for-wound-irrigation/. Accessed February 10, 2017
21. Kim P, Attinger C, Crist B, et al. Negative Pressure Wound Therapy with Instillation: Review of Evidence and Recommendations. Wounds. 2015; 27(12):S2-S19.
22. Wolvos T. Wound Instillation — The Next Step in Negative Pressure Wound Therapy. Lessons Learned from Initial Experiences. Ostomy Wound Manage. 2004; 50(11):56-66.