
Marc R. Matthews, MD is board certified in general surgery and surgical critical care by the American College of Surgeons. He has published over 50 papers in burns, trauma and surgical diseases as well as having given many national presentations. Since his arrival at the Arizona Burn Center he has concentrated on the development of telemedicine for the delivery of burn care throughout the entire state of Arizona as well as the development of disaster preparedness. He is an associate clinical professor at the University of Arizona, Creighton University, Midwestern University and AT Still Schools of Medicine. A native of California, Dr. Matthews received his medical degree from the University of California, Los Angeles, School of Medicine. Dr Matthews is a consultant for 3M.

Dr. Fernandez is a Clinical Professor of Surgery and Family Practice at the University of Texas Health Center at Tyler. Dr. Fernandez obtained his residency training at Loyola University, the University of Illinois, the University of Chicago and Northwestern University, Chicago, Illinois, with special training in trauma and burns at Kings County Hospital, SUNY Down State System, Brooklyn, New York. He is well published in multiple areas of research both in peer-reviewed articles and book chapters, and has made numerous oral and poster presentations at national and international conferences. Dr Fernandez is a consultant for 3M.
Dr. Ferrari is a Fellow in burn surgery at The Arizona Burn Center in Phoenix, Arizona
Matthews_Current Dialogues in Wound Management_2020_Article_20
INTRODUCTION
The acute care surgeon manages trauma, burn, and emergency general surgery wounds. Patients may initially start with an acute wound which evolves into a chronic wound in various stages of healing. The classic surgical technique is an operating theater visit for sharp, mechanical debridement combined with appropriate antibiotics; this is still the gold standard in the treatment of necrotic, thermally-injured or infected tissue.1 It is a challenge to take an acutely ill patient with comorbidities such as cardiovascular disease, diabetes, hypertension, chronic obstructive pulmonary disease, renal or liver failure to the operating room for sharp surgical debridement. There must be clinical assurances that these patients will survive multiple debridements and procedures. They may not be candidates for such repeated operations because of their concomitant risk of death or complications due to blood loss, general anesthetics, hemodynamic shifts or the inability to be extubated post-operatively. There may also be delays in operating room scheduling, no operating room availability, or consent issues. Modern technology has developed other treatment options to assist the surgeon or wound care provider. This is where the negative pressure wound therapy with irrigation and dwell time (NPWTi-d) becomes valuable but does not replace the surgical options.2
Wound Cleansing
Wound cleansing is a well described and utilized practice to assist with wound management.3 In lieu of the scalpel, wound cleansing removes necrotic slough, fibrinous products, cellular debris, proinflammatory mediators and prokaryotic organisms that can inhibit wound healing and subsequent wound closure.4 Normal saline is the most frequently used cleansing solution. Antimicrobial instillation fluids with a repeated delivery nurture the complex wound bed through reduction of bioburden and proinflammatory mediators, the wound progresses from the inflammatory to the proliferative stage of granulation tissue and total circumferential wound bed contraction.5,6 Antimicrobials such as Dakin’s (hypochlorite acid) solution, (Century Pharmaceuticals Inc, Indianapolis, IN);6 Vashe™ Wound Solution (hypochlorous acid) (Urgo/Steadmed, Inc, Fort Worth, TX), or sulfamylon (5% Mafenide acetate) solution (Mylan Pharmaceuticals, Inc., Canonsburg, PA) have been used.
V.A.C. VERAFLO™ Therapy
V.A.C. VERAFLO™ Therapy cleanses the wound bed through instillation of a topical wound solution with a user specified dwell time followed by defined periods of negative pressure to help remove the solubilized wound exudate and debris.7 V.A.C. VERAFLO™ Therapy use in conjunction with oral or intravenous antibiotic therapy and the necessary microstrain and macrostrain inherent within the negative pressure cycle of NPWTi-d can help remove infectious material from the wound, promote the development of granulation tissue, and may help reduce bacterial counts through cyclic delivery of topical wound solutions and repeated removal via negative pressure.8 Through macrostrain, the foam dressing draws the wound edges together, reduce edema, promote perfusion and remove infectious material.9 Tissue micro-deformation from the microstrain leads to cellular stretch which stimulates cellular activity and granulation tissue development. Alternating cyclical irrigation rotations cleanse the wound bed to prepare it for closure or skin grafting.10
V.A.C. VERAFLO CLEANSE CHOICE™ Dressing
After initial mechanical debridement in the operating room or clinic, the wound length, width and depth are assessed. Once hemostasis has been achieved and the wound irrigated, the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing can be applied to the wound bed. This dressing removes thick exudate such as slough, fibrinous material, cellular breakdown products, metabolic proinflammatory products, prokaryotic organisms and debris into the larger through holes.11 It has a reticulated open-cell foam contact layer with through holes 1-cm in diameter uniformly interspersed 0.5-cm apart and designed to be placed directly against the wound bed. During NPWTi-d, these larger holes facilitate the removal of small and larger particulate matter when the foam is changed every 48- to 72-hours.12 Each dressing kit comes with two additional foams with different thicknesses (1.6-cm and 0.8-cm) and without through holes. These two layers of foam dressing have interstices that are 400 to 600 microns in width for an even displacement of negative pressure to draw fluid out of the wound bed. They are hydrophilic and lack the hydrophobicity seen with the previously created negative pressure dressings. One or both foam layers can be placed over the wound contact foam to fill the patient’s wound cavity. The wound is then covered with either a V.A.C.® Advance Drape or the recently developed DERMATAC™ Drape to create a seal. While other consensus panels recommend framing the wound prior to application, this is not necessary if an adequate seal is initially created that holds suction.13 We recommend the use of skin preparation products (such as DuoDerm® [ConvaTec, Oklahoma City, OK] or Mastasol®Liquid Adhesive [Eloquest Healthcare, Ferndale, MI]) to protect the periwound skin from leakage, and provide a tight seal for NPWT and/or instillation.
V.A.C.ULTA™ Therapy Unit
With the instillation of fluid over the wound bed, the V.A.C.ULTA™ Therapy Unit controls wound cleansing in a regular timed cyclical fashion. The advantage with this system is that the wound can be irrigated 24 times in 72 hours if the negative pressure cycle is set for 3 hour increments. We determine the amount of instillation fluid needed to cover the wound bed by multiplying the wound width (cm) by the length (cm) and depth (cm) of the wound. This volume is multiplied by the coefficient of 0.2 to give the calculated amount needed.14 Another way to determine the volume to be instilled is by using the “Fill-Assist” option on the V.A.C. ULTA™ device.
As programmed, every three hours the V.A.C.ULTA™ Therapy Unit will deliver a set amount of topical wound solution for a set amount of time to soak the wound bed before it is removed with loosened or solubilized exudate and debris. Another feature that must be considered is the length of fluid instillation time. There is no specific time period, but the instillation frequency should be determined by the need for the wound bed cleansing. For this reason, an instillation cycle every 3 to 6-hours would be appropriate. While -125 mmHg is regarded as the default setting, -75 mmHg and lower can be enough to remove fluid from the wound; although there is no empiric data available in the literature outside of consensus statements.13 In addition, dwell time length can vary from one minute to thirty minutes; no studies for dwell time have been conducted.
V.A.C. VERAFLO CLEANSE CHOICE™ Dressing Use is NOT RECOMMENDED in these Circumstances
While NPWTi-d may be necessary to assist with wound bed preparation, some clinical scenarios are contraindicated for its use. Exposed and unprotected internal organs or anastomotic sites, unexplored tunnels, exposed nerves or blood vessels, necrotic tissue with eschar are contraindicated for NPWTi-d use. V.A.C. VERAFLOTM Therapy is intended for use with topical wound solutions and suspensions. Only use fluids indicated for wound treatment and review the solution manufacturer’s instructions for use prior to instillation. Additionally, only use wound solutions compatible with V.A.C. VERAFLOTM Dressings and disposable components. Contact your 3M representative for a list of compatible solutions.
V.A.C. VERAFLOTM Therapy is not intended for use with cellular or acellular bioengineered tissues, V.A.C.® GRANUFOAM SILVERTM Dressings, PREVENATM Incision Management Dressings, ABTHERATM SENSAT.R.A.C.TM Open Abdominal Dressing, or KCI negative pressure wound therapy gauze dressings.
Do not use V.A.C. VERAFLOTM Dressings with Octenisept, hydrogen peroxide or solutions that are alcohol-based or contain alcohol. Do not deliver fluids to the thoracic or abdominal cavity due to potential risk to alter core body temperature and potential for fluid retention in the cavity. Do not use V.A.C. VERAFLOTM Therapy unless the wound has been thoroughly explored due to the potential for inadvertent instillation of topical wound solutions.
Use of V.A.C. VERAFLO™ Therapy with V.A.C. VERAFLO CLEANSE CHOICE™ Dressing in Three Cases
Irrespective of the type of topical wound solution, the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing is a necessary foam for the delivery of wound bed irrigation. Three cases are presented where V.A.C. VERAFLO CLEANSE CHOICE™ Dressing and V.A.C. ULTATM Therapy Unit were used to heal a variety of wounds. Study approval was obtained from the Institutional Review Board at Valleywise Health Medical Center. Written informed consent was obtained for all patients.
Case 1
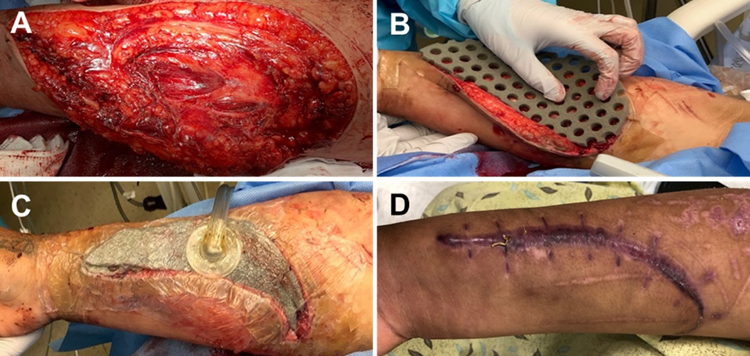
A 19-year-old female presented for care eight hours after a house fire with a 6% total body surface area burn injury to the face, left upper extremity and a right forearm laceration (20 x 8 cm) (Figure 1a). Following debridement, V.A.C. VERAFLO™ Therapy with V.A.C. VERAFLO CLEANSE CHOICE™ Dressing was placed over the right forearm wound and instillation using Vashe™ Wound Solution (45 cc’s with a 15-minute dwell time followed by 3 hours of continuous negative pressure at -125 mmHg) was initiated because the wound was open for eight hours (Figure 1b and 1c). Dressing changes occurred every 48 hours. V.A.C. VERAFLO™ Therapy was discontinued on hospital day (HD) 4, followed by surgical closure of the right forearm wound and autografting operation for the left forearm wound (not pictured). The patient was discharged on HD 12 to an acute care rehabilitation hospital and followed in clinic for post-operative care (Figure 1d).
Case 2
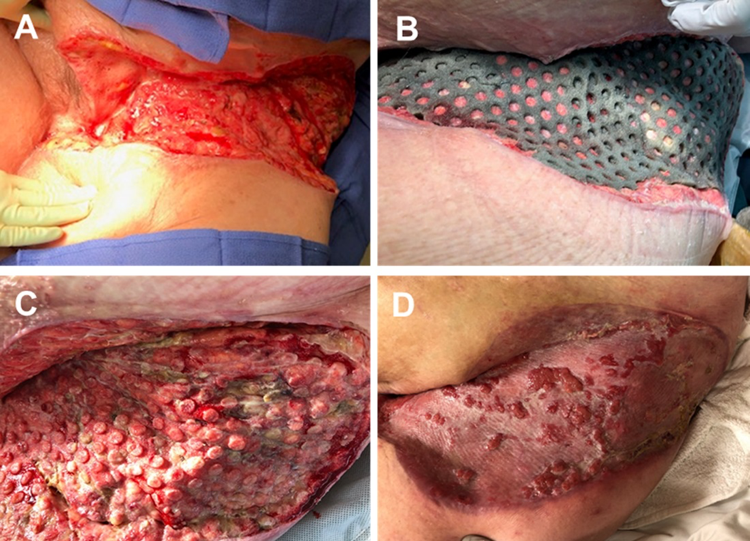
A 59-year-old diabetic, hypertensive and morbidly obese female developed pain and erythema in her left inguinal and lower abdominal area. Computerized tomographic scan revealed air and fluid in the perineal, lower abdominal wall and inguinal regions. She was diagnosed with necrotizing fasciitis. With intravenous antibiotics initiated due to positive bacterial culture results, the patient underwent seven excisional debridements by HD 18 (Figure 2a). V.A.C. VERAFLO™ Therapy with V.A.C. VERAFLO CLEANSE CHOICE™ Dressing was utilized between the first and third sharp debridement procedures with irrigation utilizing 100 cc of hypochlorous acid (VasheTM Wound Solution) at 100 cc for a 20-minute dwell time with three hours NPWT at -125 mmHg. NPWT was used for 8 days with dressing changes every 72 hours (Figures 2b and 2c). After 6 days, V.A.C. VERAFLO™ Therapy with the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing cover layer was used to smooth out the columnar macrodomes and provide a smooth granulated wound bed before skin grafting (Figures 2b and 2c) at -125 mmHg. The patient received a split thickness skin graft on HD 24 and was discharged on HD 36 for clinic follow-up.
Case 3
While cooking with oil, a 54-year old male sustained a 4% TBSA full-thickness burn to his right thigh, knee and leg (Figure 3a). He was taken to the operating room on HD 2 for tangential excision of his right lower extremity burns through to the subcutaneous tissue (Figure 3b). To facilitate granulation tissue growth, V.A.C. VERAFLO™ Therapy using V.A.C. VERAFLO CLEANSE CHOICE™ Dressing was applied starting on HD 4 utilizing 50 cc of hypochlorous acid (VasheTM Wound Solution) with a 20-minute dwell time followed by three hours of NPWT at -125 mmHg. This was conducted after each repeat tangential excision of the wound. Dressing changes occurred every 48 to 72 hours. The wound was again debrided on HD 10 (Figure 3c) and HD 13 (Figure 3d). After split-thickness skin graft coverage, the wound was covered with Mepitel™ (Mölnlycke, Gothenburg, Sweden) followed by application of V.A.C.® Therapy as a bolster at -125 mmHg. The patient had a total of 16 days of NPWT, which was removed on HD 20 (Figure 3e). The patient was discharged to a skilled nursing facility with follow-up in the burn clinic.

CONCLUSION
Mechanical debridement combined with appropriate antibiotics is the gold standard in the treatment of necrotic, thermally injured or infected tissue. However, these patients may not be candidates for such repeated operations due to the concomitant risk of death or other complications. Additionally, external factors such as operating room scheduling or operating room availability can create a delay in the patient undergoing these sharp debridement procedures. In our experience, V.A.C. VERAFLO™ Therapy with V.A.C. VERAFLO CLEANSE CHOICE™ Dressing can assist with wound cleansing between operative debridements while the patient remains in the intensive care unit or hospital wards.
Patient data and photos courtesy of Marc Matthews, MD, FACS, FASGS.
As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
NOTE: Specific indications, contraindications, warnings, precautions and safety information may exist for these products. Please consult a healthcare providers and product instructions for use prior to application. Rx only.
References
- Wolcott RD, Kennedy JP, Dowd SE. Regular debridement is the main tool for maintaining a healthy wound bed in most chronic wounds. J Wound Care 2009;18(2):54-56.
- Teot L, Boissiere F, Fluieraru S. Novel foam dressing using negative pressure wound therapy with instillation to remove thick exudate. Int Wound J 2017;14(5):842-848. doi:10.1111/iwj.12719.
- Kim PJ, Applewhite A, Dardano AN et al. Use of a novel foam dressing with Negative Pressure Wound Therapy and Instillation: Recommendations and clinical experience. Wounds 2018;30(Suppl 3):S1-S17.
- Wheeler CB, Rodeheaver GT, Thacker JG, Edgerton MT, Edlich RF. Side-effects of high pressure irrigation. Surg Gynecol Obstet 1976;143(5):775-778.
- Gabriel A. Integrated negative pressure wound therapy system with volumetric automated fluid instillation in wounds at risk for compromised healing. Int Wound J 2012;9(Suppl 1):25-31.
- Yang C, Goss SG, Alcantara S, Schultz G, Lantis Ii JC. Effect of Negative Pressure Wound Therapy With Instillation on Bioburden in Chronically Infected Wounds. Wounds 2017;29(8):240-246.
- Lessing C, Slack P, Hong KZ, Kilpadi D, McNulty A. Negative pressure wound therapy with controlled saline instillation (NPWTi): dressing properties and granulation response in vivo. Wounds 2011;23(10):309-319.
- Goss SG, Schwartz JA, Facchin F, Avdagic E, Gendics C, Lantis JC, II. Negative Pressure Wound Therapy with Instillation (NPWTi) Better Reduces Postdebridement Bioburden in Chronically Infected Lower Extremity Wounds than NPWT Alone. Journal of the American College of Clinical Wound Specialists 2014;4(4):74-80.
- Saxena V, Hwang CW, Huang S, Eichbaum Q, Ingber D, Orgill DP. Vacuum-assisted closure: microdeformations of wounds and cell proliferation. Plast Reconstr Surg 2004;114(5):1086-1096.
- McNulty A, Spranger I, Courage J, Green J, Wilkes R, Rycerz A. The consistent delivery of negative pressure to wounds using reticulated, open cell foam and regulated pressure feedback. Wounds 2010;22(5):114-120.
- Kim PJ, Attinger CE, Steinberg JS et al. The impact of negative-pressure wound therapy with instillation compared with standard negative-pressure wound therapy: a retrospective, historical, cohort, controlled study. Plast Reconstr Surg 2014;133(3):709-716.
- Gupta S, Gabriel A, Lantis J, Teot L. Clinical recommendations and practical guide for negative pressure wound therapy with instillation. Int Wound J 2016;13(2):159-174.
- Kim PJ, Attinger CE, Constantine T et al. Negative pressure wound therapy with instillation: International consensus guidelines update. Int Wound J 2020;17(1):174-186.
- McKanna M, Geraci J, Hall K et al. Clinician panel recommendations for use of negative pressure wound therapy with instillation. Ostomy Wound Manage 2016;(Suppl):3-14.
© 2020 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. PRA-PM-US-02697 (09/20).

