Cindy has been a Registered Nurse since 1978. For the past 26 years, Cindy has worked in various sales, clinical, marketing as well as research and development roles at KCI. For 2 years (2009-2011) she devoted her energies to the launch of V.A.C. Therapy in Japan, India and China, where she educated KCI’s sales force and lectured at major universities across those countries. Cindy is the senior author of 2 posters that have been presentated at international and national wound care conferences She is currently the Senior Director of Clinical Science and Education at KCI Corporate Headquarters and lectures extensively in the U.S. and abroad on the entire portfolio KCI has to offer.
Miller-Mikolajczyk_Current Dialogues in Wound Management_2019_Special Spring Edition
INTRODUCTION
Anyone who has ever undertaken a new cooking recipe, and who desires an optimal outcome, typically follows the written ingredient amounts and method/timing of cooking. This ensures the best chance for a successful outcome. Once that recipe has been validated, small tweaks can be made to customize the recipe to alter the outcome. Use of negative pressure wound therapy (NPWT) with instillation and dwell time (NPWTi-d) can be viewed in much the same manner once an appropriate patient has been identified, especially for clinicians who have not yet gained experience with it. There are a few basic steps to using NPWTi-d that, if followed, may help increase the likelihood of a positive experience for the patient.
Use of NPWT for wound management is well established in the literature as well as in clinical practice. The addition of an instilled topical wound solution with dwell time, which alternates with negative pressure wound therapy, facilitated wound cleansing that helped promote wound healing.1-3 Compared with standard NPWT, NPWTi-d involves the use of unique dressing options as well as knowledge of how to access and use the instillation-specific pump program, which allows the automated, volumetric delivery of topical wound solutions. These changes in practice from standard NPWT are important for clinicians to understand when being introduced to NPWTi-d. While some clinicians who are experienced with NPWTi-d employ advanced features to match various wound characteristics,4 other experienced clinicians prefer to stick with the basics of the therapy.
The purpose of this article is to describe, in simplified steps (a “recipe”, if you will), how to apply NPWTi-d to an appropriate patient using basic therapy unit settings, topical wound solutions, and components. Following these steps may help optimize the use of the therapy in most appropriate wounds and help increase the clinician’s comfort level when instituting this therapy. The recommendations here are based on clinical experience and published evidence of best practices.
Once the wound has been thoroughly assessed and it has been established that the wound is indicated and not contraindicated for the use of NPWTi-d, the following steps can be instituted along with the products’ instructions for use. Prior to applying the therapy, the patient and wound bed should be adequately prepared using good wound care principles.10 A prescription is required to start NPWTi-d.
STEPS FOR APPLYING NPWTI-D
1. Gather all needed components:
•V.A.C.ULTA™ Therapy Unit
•V.A.C.ULTA™ Canister
•VERALINK™ Cassette
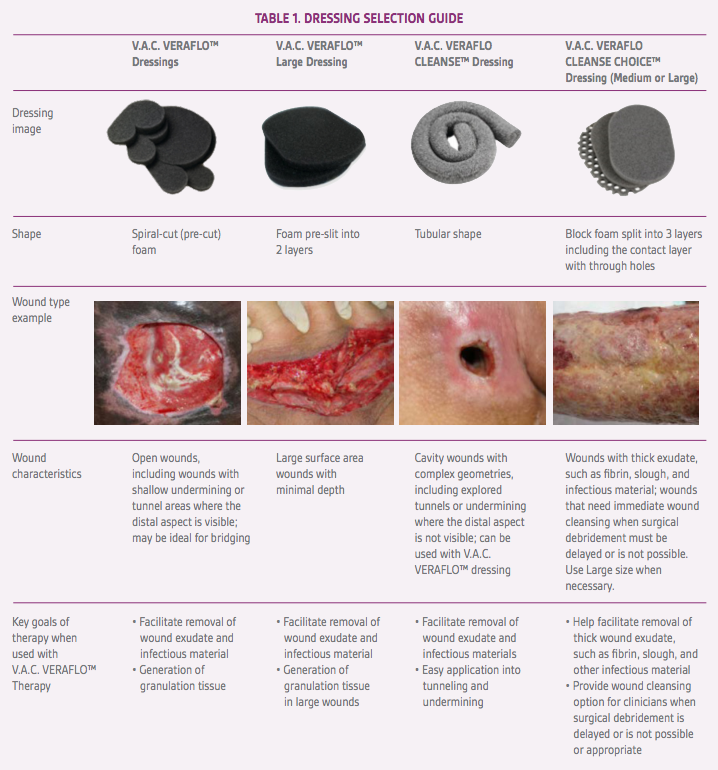
•V.A.C. VERAFLO™ Dressing Kit of clinician’s choice (Table 1)– Medium or large dressing (V.A.C. VERAFLO™ Dressing, V.A.C. VERAFLO CLEANSE™ Dressing or V.A.C. VERAFLO CLEANSE CHOICE™ Dressing)
•V.A.C.VERAT.R.A.C.™ Pad with tubing (included in dressing kit) – V.A.C. VERAT.R.A.C.™ Pad included in Medium dressing kit– V.A.C. VERAT.R.A.C.™ DUO Tube Set included in large dressing kit– DUO Tube Sets are also available separately
•3M™ Cavilon™ No Sting Barrier Film wipes (included in dressing kit)
•V.A.C.® Advanced Drape (included in dressing kit)•Manufacturer’s approved topical wound solution of clinician’s choice (Table 2)
2.Assemble the system
a.Attach VERALINK™ Cassette to side of V.A.C.ULTA™ Unit.
b.Raise solution container arm and rotate 180 degrees. Lock into place.
c.Clamp tubing on solution tubing.
d.Spike solution bag and hang on hanger arm.
e.Do not prime the system with the topical solution as the system will do this automatically.
f.Tuck bag inside the VERALINK™ Cassette when necessary.
g.Attach the canister to the right side of V.A.C.ULTA™ Unit.
Caution: The listing of the above solutions is neither an endorsement nor an indication of a solution’s clinical efficacy. These solutions are included based on KCI in-house testing of disposables, mechanical properties, biocompatibility, and solution interaction and found to be compatible with the V.A.C.ULTA™ Therapy System components. If wound healing goals are not being achieved, consider an alternate instillation frequency, solution concentration, or solution type deemed appropriate by a physician. Please follow solution manufacturer’s Instructions for Use prior to use with V.A.C. VERAFLO™ Therapy.Dermacyn® and Microcyn® are trademarks of Sonoma Pharmaceuticals (Petaluma, CA). Sulfamylon® is a trademark of Mylan Institutional Inc. (Rockford, IL). Prontosan® is a trademark of B. Braun Medical, Inc. (Bethlehem, PA). Vashe® is a trademark of SteadMed Medical (Fort Worth, TX). Puracyn® is a trademark of Innovacyn, Inc. (Rialto, CA). NeutroPhase® is a trademark of NovaBay Pharmaceuticals, Inc. (Emeryville, CA).
3.Apply the dressing
a.Wipe the periwound area with 3M™ Cavilon™ No Sting Barrier Film, as needed.
b.In hard-to-seal locations, consider applying drape strips around the wound in windowpane fashion.
c.Assess wound dimensions.
d.Protect sensitive structures, vessels, and organs.
e.Cut foam to fit wound dimensions and place into wound cavity ensuring direct contact with all surfaces of the wound, including tunnels and undermining. Keep count of all foam pieces placed in the wound and record on drape and in patient record, as per facility protocol. – Dressing foam types can be used in combination as appropriate. – Refer to Instructions for Use for detailed information on applying each dressing type.
f.Apply V.A.C.® Advanced Drape to cover wound plus 3-5 cm of intact skin.
g.Cut 2.5 cm diameter hole in V.A.C.® Advanced Drape.
h.Apply VERAT.R.A.C.™ Pad over hole(s) in the drape.
4.Connect dressing tubing to device
a.Connect appropriate VERAT.R.A.C. DUO™ Tube to the canister tubing to allow for negative pressure application and solution removal.
b.Connect the small lumen VERAT.R.A.C. DUO™ Tube to V.A.C. VERALINK™ Cassette tubing to allow for solution delivery. Be sure the connection is secure.
c.Ensure all white tubing clamps are open.
5.Choose device settings
a.Choose V.A.C. VERAFLO™ Therapy program from the touch screen.
b.Select “OK” to use default settings for therapy.Default settings are:
a. Fill Assist (ON)
b. Start Phase (Instill)
c. Soak Time (10 minutes)
d. V.A.C.® Therapy Time (3.5 hours)
e. Target Pressure (-125 mmHg) f. Intensity (Low)
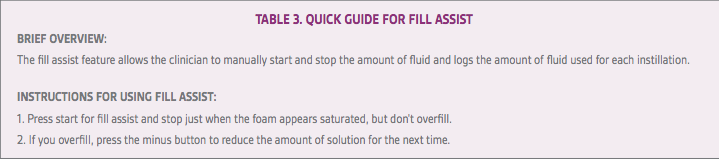
c.Use fill assist tool to determine solution volume; don’t overfill (Table 3)
6.Check that therapy is activated
•Start therapy.
•The foam will draw down while the therapy unit performs a seal check. This may take a few minutes, depending on the size of wound and presence of microleaks.
•Make sure the dressing has wrinkled appearance after therapy is initiated and that there are no hissing sounds or other evidence of leaks.The SEAL CHECK™ Feature will assist the clinician in this important step.
CONCLUSION
Compared with standard NPWT, use of NPWTi-d involves unique dressing options as well as accessing and using the instillation-specific pump program. A firm understanding of these changes in workflow required with use of NPWTi-d is important for any clinician using the therapy. However, when it comes to choosing configurations and settings for the NPWTi-d system, starting with basic therapy settings, topical wound solutions and components may offer the best recipe for success with appropriate patients, especially for clinicians who are new to the therapy. The simplified steps outlined in this article may be used as a guide to optimize use of the topical wound instillation therapy in most appropriate wounds, increasing the likelihood of a positive patient and clinician experience.
References
1.Ludolph I, Fried FW, Kneppe K, Arkudas A, Schmitz M, Horch RE. Negative pressure wound treatment with computer-controlled irrigation/instillation decreases bacterial load in contaminated wounds and facilitates wound closure. Int Wound J. 2018;15(6):978-984. doi: 10.1111/iwj.12958.
2.Anghel EL, Kim PJ, Attinger CE. A solution for complex wounds: the evidence for negative pressure wound therapy with instillation. Int Wound J. 2016;13 Suppl 3:19-24. doi: 10.1111/iwj.12664.
3.Gabriel A, Kahn K, Karmy-Jones R. Use of negative pressure wound therapy with automated, volumetric instillation for the treatment of extremity and trunk wounds: Clinical outcomes and potential cost-effectiveness. Eplasty. 2014;14:e41.
4.Yang C, Goss SG, Alcantara S, Schultz G, Lantis Ii JC. Effect of negative pressure wound therapy with instillation on bioburden in chronically infected wounds. Wounds. 2017;29(8):240-246.
5.Kim PJ, Attinger CE, Oliver N, et al. Comparison of outcomes for normal saline and an antiseptic solution for negative-pressure wound therapy with instillation. Plast Reconstr Surg. 2015;136(5):657e-664e. doi: 10.1097/PRS.0000000000001709.
6.Fluieraru S, Bekara F, Naud M, et al. Sterile-water negative pressure instillation therapy for complex wounds and NPWT failures. J Wound Care. 2013;22(6):293-299.
7.Brinkert D, Ali M, Naud M, Maire N, Trial C, Téot L. Negative pressure wound therapy with saline instillation: 131 patient case series. Int Wound J 2013;10 Suppl 1:56-60. doi: 10.1111/iwj.12176.
8.McKanna M, Geraci J, Hall K, et al. Clinician panel recommendations for use of negative pressure wound therapy with instillation. Ostomy Wound Manage. 2016;62(4):S1-S14.
9.Kim PJ, Attinger CE, Crist BD, et al. Negative pressure wound therapy with instillation: review of evidence and recommendations. Wounds. 2015;27(12):S2-S19.
10.Snyder RJ, Fife C, Moore Z. Components and quality measures of DIME (devitalized tissue, infection/inflammation, moisture balance, and edge preparation) in wound care. Adv Skin Wound Care. 2016;29(5):205-215. doi: 10.1097/01.ASW.0000482354.01988.b4.