Dr. Jodee Brown obtained her doctoral degree from Barry University’s School of Podiatric Medicine and Surgery. She also holds a Master’s degree in Health Management and is currently a 3rd year chief resident at Jackson North Medical Center.

Dr. Kellee Campbell is a graduate of Barry University’s School of Podiatric Medicine and is currently completing her podiatric medical and surgical residency training at Northwest Medical Center where she serves as the chief resident.
Brown and Campbell_Current Dialogues in Wound Management_2016_Volume 2_Issue 1
INTRODUCTION
The provision of medical care starts with diagnosis and ends with the administration of treatment. From this simplified logic, health care necessitates team activity that involves different health professionals to systematically identify a health disorder and render the appropriate treatment.
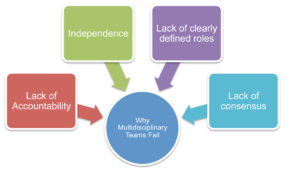
According to Moore et al, a multidisciplinary team involves a group of healthcare workers from various disciplines, independently providing specific services to the patient.1 Ideally, a multidisciplinary team provides well-rounded care, as compared to the limited role of an individual physician, and can utilize the resources needed to meet the high demands of patients. If this approach is properly executed, the result has favorable measurable outcomes.2 Though the multidisciplinary team approach has been proven efficacious, achieving a successful model is often difficult for health professionals. This article seeks to examine several key reasons why these teams fail to achieve the ideal multidisciplinary model.
LACK OF CONSENSUS
Multidisciplinary teams are composed of members from various disciplines such as nurses, social workers, dieticians, health educators, and physicians among others. This diverse pool of medical personnel increases the amount of talent available for collaboration of ideas and a smoother transition for the patient from diagnosis to treatment to follow up care. When forming a team, it is important to assign responsibilities to individuals and define their roles to avoid conflict and duplication of duties.2 Members of different disciplines may have distinct roles in the healthcare sector, but in the team approach, some roles may overlap and create discord among the group. Communication is key and egos must be left at the door for the wellbeing of the patient and the betterment of the team. Take, for instance, a consulting physician making a judgment call on a patient and prescribing a medication of which the admitting physician does not approve. Without proper communication, this can lead to a lack of trust on the part of the admitting doctor, and a fear of conflict from consulting physicians, seeking artificial harmony over constructive, passionate debate.3This lack of trust among team members lays the foundation for potential dysfunction, leading ultimately to more costly and inferior patient outcomes due to a waste of time, energy, and resources.
LACK OF CLEARLY DEFINED ROLES
Another major reason the multidisciplinary approach fails is due to the lack of clear guidelines on the role of each team player.5Lack of documented and precise roles of each member also threatens the survival of the team due to resulting conflicts, and ultimately to a lack of commitment among its members. A team that has no clear direction cannot fully commit to the task at hand and thereby fosters a disharmonious environment.3,7 This, therefore, necessitates the defining of roles and responsibilities upon formation of the teams. Moreover, when building a team, one must first take inventory of the group and discover who wants to lead and who wants to be led.4This simple process can ensure coordination of efforts and efficiency in healthcare provision.
LACK OF ACCOUNTABILITY
The scope of practice relates to the procedures, processes and actions permitted to a healthcare provider while keeping within terms of the profession. One cannot build a successful team if group members are not confident in their individual roles. Every member needs to know the extent of their operations to pave the way for other members to play their roles. Without this, confusion, duplication of tasks and an absence of liability result. A greater burden is thusly placed on the team leader when discord arises. Team members that are unaccountable have no clear standards of care or performance, and mediocrity is often the result.3,6 Consider the old “a chain is only as strong as its weakest link” analogy; through proper support and communication weaker links can be strengthened and stronger links won’t have to be over stressed. Every link has its role to play in strengthening the chain without excessively infringing on the duties of the others. The roles of each member, therefore, need to be addressed and communicated to the group to ensure the smooth flow of operations conducted by the team.
INDEPENDENCE
“Not finance. Not strategy. Not technology. It is teamwork that remains the ultimate competitive advantage, both because it is so powerful and so rare.”3 It is important not only to understand why teams fail, it is also important to understand where teams fail, and it starts with the individual. Every healthcare professional has a different culture in which they operate. These cultures have gradually evolved over time, reflecting various factors, including codes of conduct and even gender issues.8 In addition, individuals seeking a career in the medical profession are encouraged to be competitive. This aggressive and strong-minded environment, coupled with the professional culture students are exposed to, sets the framework for many medical professionals to adopt an individualistic approach.7,8 Students must prove they are better, smarter, and have a greater skill set than their peers to obtain the best position or the highest salary. This independent ideology often follows the student into their professional life, and to some extent, it negates any effort for teamwork and collaboration.
CONCLUSION
A multidisciplinary approach to health care is one that is proven to have better outcomes, higher patient satisfaction, and an improved quality of life.1,2,5 The discrepancies emerging from the lack of clearly defined roles, trust, ego, and a discordance between specialties results in the failure of teams. Moreover, there is a need for further education and training of healthcare providers, placing greater emphasis on communication, collaboration and confidence in colleague, while encouraging healthy debate and accountability. According to Lencioni, “Teamwork ultimately comes down to practicing a small set of principles over a long period of time. Members of functional teams overcome the natural tendencies that make trust, conflict, commitment, accountability, and a focus on results so elusive.”
References
1.Moore Z, Butcher G, Corbett LQ, et al. AAWC, AWMA, EWMA Position Paper: Managing Wounds as a Team. J Wound Care. 2014; 23 (5 Suppl.): S1–S38.
2.Codispoti C, Douglas MR, McCallister T, et al. The use of a multidisciplinary approach to improve glycemic control and quality of life by the prevention of complications among diabetic patients. J Okla State Med Assoc. 2004 May: 97 (5):201-4.
3.Lencioni P. The five dysfunctions of a team. John Wiley & Sons. 2006.
4.Jungyai K, Bailey Kloch M, Kim K. Interprofessional experiences and attitudes toward interprofessional health care teams among health sciences students. Social Work in Health Care. 2014: 53 (6);552-567.
5.Collin K, Valleala U, Herranen S, et al. Ways of interprofessional collaboration and learning in emergency work. Studies in Continuing Education. 2012: 34 (3); 281-300.
6.Mitchell M, Wynia R, Golden B, et al. Core Principles & Values of Effective Team-Based Health Care, Institute of Medicine, 2014. [Online]. Available at: www.iom.edu/tbc.
7.Boulton AJM, Cavanagh P, Rayman G. The foot in diabetes. 4thed. Chester, West Sussex John Wiley & Sons; 2006.
8.Kvarnström S. Difficulties in collaboration: A critical incident study of interprofessional healthcare teamwork. Journal of Interprofessional Care. 2008:22 (2); 191-203.
9.Hall P. Interprofessional teamwork: professional cultures as barriers. Journal of Interprofessional care. 2005: 19 (1) 188 – 196