
Dr. Johnson is doubly certified by both the American Board of Surgery and American Board of Plastic Surgery. He is a Fellow of the American College of Surgeons and a member of the American Society of Plastic Surgeons. Dr. Johnson trained in surgery and helped care for battle-injured soldiers where he developed a passion for the reconstructive surgeries done to treat their devastating wounds. He was a general surgeon for 2 years and deployed to Afghanistan with a small team in austere and dangerous environments. Ultimately, he returned to Baltimore to train under leaders in plastic surgery where he learned microvascular free tissue transfer, hand surgery, treatment of congenital and acquired craniofacial deformities, and cosmetic surgery. Dr. Johnson studied at Johns Hopkins University for his fellowship where he gained subspecialty expertise in rhinoplasty and nasal reconstruction, facial reanimation, head & neck microsurgery, Mohs reconstruction, ear reconstruction, and craniomaxillofacial trauma. Dr Johnson is a consultant for KCI.
Johnson_Current Dialogues in Wound Management_2020_Article_10
CONCEPT AND APPLICATIONS
Closed incisional negative pressure therapy (ciNPT) may reduce disruptive shear forces and serve as an antibacterial barrier over a clean, closed surgical wound. Our observation has been that ciNPT is associated with fewer complications such as seroma, dehiscence, surgical site infection, pain, and soft tissue necrosis. At our institution for the past four years, we have considered ciNPT for any breast reconstruction case with higher-than-normal-risk for developing postsurgical complications, in which:
1. Incisional healing requires overcoming a moderate-to-high degree of tension
2. The operation requires significant undermining or dissection that compromises vascularity
3. The patient has a medical or an anatomic risk factor that significantly increases risk
4. The selected operation has a historically high complication rate despite best practices
5. The consequences of a complication are devastating, such as implant exposure after mastectomy flap necrosis.
The PREVENA RESTOR BELLA•FORM™ Incision Management System is a wide-area form of ciNPT designed to protect and stabilize tissue, reduce edema, and manage the incision plus the surrounding soft tissue envelope. This expanded area might be devascularized more than a standard surgical wound due to the necessary dissection, such as after a nipple-sparing mastectomy (NSM).
I particularly favor the PREVENA RESTOR BELLA•FORM™ System when performing immediate implant-based breast reconstructions (especially after NSM, direct-to-implant, and/or prepectoral technique with thin skin), large-volume reductions (especially when a Wise pattern skin incision is used), and gender-affirming chest surgery. I have found that the PREVENA RESTOR BELLA•FORM™ System is helpful on high-tension mastectomy and as a bolster over free nipple grafts as well as augmentation with a large implant under tight skin. Additionally, I consider its use after post-bariatric reduction or mastopexy when combined with abdominoplasty, large-implant cosmetic augmentation if the patient opts for it, and revision surgeries with complex scars or pedicle anatomy. A challenging immediate bilateral breast reconstruction case is described to illustrate the utility and potential benefit of the PREVENA RESTOR BELLA•FORM™ System.
Patient presentation
A 48-year-old female presented with a palpable 2 cm left breast retroareolar infiltrating ductal carcinoma at the 1 o’clock position and a clinically negative axilla. Due to the tumor’s location, a traditional left mastectomy (non-nipple-sparing) with left sentinel lymph node biopsy was planned. Genetic testing was negative for BRCA, but the patient had a significant family history of breast cancer in maternal relatives and desired contralateral prophylactic NSM.
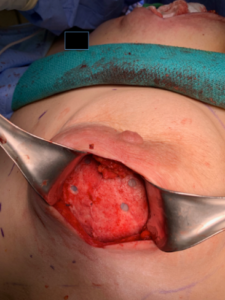
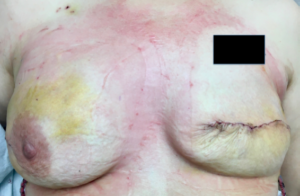
The patient’s medical and anatomic risk factors included a history of weight fluctuations, skin laxity with striae, thin soft tissue envelope, former tobacco use status, grade 2 breast ptosis, and asymmetry (Figure 1). She desired reconstructions that resulted in larger volume and improved shape of both breasts.

Options for the right breast reconstruction included:
• Traditional mastectomy with immediate tissue expander (TE) reconstruction followed by implant exchange and nipple reconstruction.
• First-stage mastopexy to reposition the nipple followed by second-stage prophylactic mastectomy with immediate direct-to-implant (DTI) reconstruction.
• NSM with immediate TE reconstruction and subsequent revisions to reposition the nipple as needed.
The patient opted for the third right breast reconstruction option.
Case Description
The oncologic surgeon used a transverse mastectomy incision on the left, leaving thin upper and lower mastectomy flaps. The right side was treated with a prophylactic NSM via a lateral radial incision. The immediate prepectoral reconstruction with a TE covered by human acellular dermal matrix (ADM) on the right was completed.
During the same reconstruction procedure on the left breast, the patient suddenly became hemodynamically unstable with tachycardia, hypotension, and hypoxia. Vasopressors were administered for cardiovascular support. Breath sounds were absent on the right and a chest tube was placed for presumed tension pneumothorax. Hemodynamics improved after the thoracostomy, but the patient was significantly hypertensive due to the vasopressors she had received.
In the setting of this hypertension, the patient next developed a rapidly expanding hematoma on the right side, which had already been closed. The layered incision was reopened, the wound was explored. A 300 mL hematoma was evacuated. The TE and ADM were explanted in order to fully explore the wound bed, and an actively bleeding pulsatile vessel on the undersurface of the mastectomy flap was identified and ligated. On the left breast, diffuse medical oozing was seen, but there was no surgical source of bleeding.
As the patient’s vital signs became labile, the decision was made to abandon completion of the case and expeditiously bring the patient to the intensive care unit for warming, stabilization, and workup. Sterile clean laparotomy sponges were packed into the open wounds and covered with a sterile iodophor impregnated adhesive drape dressing (Ioban™). A central venous catheter was inserted and the patient remained intubated overnight.
The clinical workup resulted in a diagnosis of right-sided tension pneumothorax from barotrauma, likely related to malposition of the endotracheal tube. Computed tomography scan ruled out bleb disease or a pulmonary embolism and the patient’s serum enzymes and echocardiogram ruled out cardiac ischemia or other pathology. Blood tests were negative for bacteremia or disseminated intravascular coagulation. By the next day, the patient was more stable and the right chest tube showed no active air leak. She was still receiving vasopressors but was being weaned. After a thorough discussion with the patient’s family and all consulting physicians, the decision was made to return to the operating room for a redo of the TE-based reconstruction versus layered closure on postoperative day one.
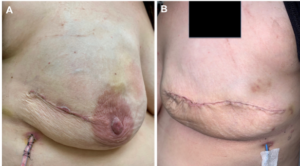
The mastectomy flaps appeared bruised, traumatized, and possibly dysvascular
(Figure 2). The tissue surfaces of both wounds were gently debrided with a cautery scratch pad and washed with a sequence of betadine solution, chlorhexidine gluconate 4% soap solution, copious amounts of sterile saline, and triple antibiotic solution. When irrigation and debridement were complete, the patient had been weaned off all vasopressors.

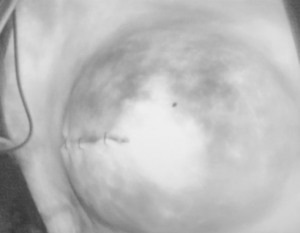
Examination and imaging with indocyanine green (ICG) laser angiography confirmed adequate perfusion to the incision edges despite the clinical appearance, soft tissue insults and vasopressor use. Medium-height TEs were implanted superficial to pectoralis major and covered anteriorly by perforated human ADM (Figure 3). Repeat ICG imaging confirmed adequate tissue perfusion after closure (Figure 4). Three layers were closed with deep absorbable monofilament and drains were placed (Figure 5).
A Cavilon™ Advanced Skin Protectant was applied on the skin of the reconstructed breasts and chest and drains were protected with a chlorhexidine gluconate impregnated dressing (Biopatch®, Ethicon, Somerville, NJ) as a protection against external sources of infection and transparent film dressings to seal the area and isolate the drain tubing from ciNPT.
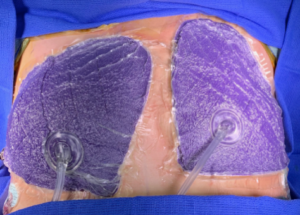
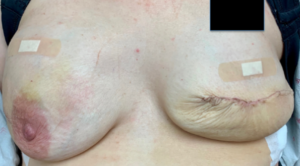
A PREVENA RESTOR BELLA•FORM™ System (size medium) was applied to both reconstructed breasts, offset slightly to avoid any overlap in the sternal midline (Figure 6). A loose surgical bra and gentle fluffy dressings were added, taking care to avoid any undue pressure.
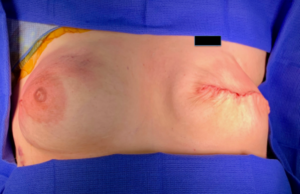
The patient was discharged to home two days later. She was given an empirical course of oral antibiotics and she returned to the office for help with PREVENA RESTOR BELLA•FORM™ System removal on day 6 after placement. Despite some bruising and skin irritation, the flaps were intact and viable (Figure 7). There was no dehiscence or necrosis. The right nipple-areolar complex was adequately preserved.
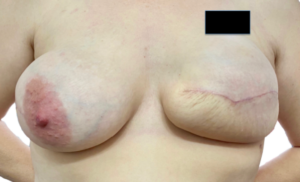
At the two-week follow-up, the skin flaps were healthy (Figure 8), the patient had not developed any infection. The drains were removed, and the TEs underwent their first round of expansion (Figure 9). The patient continued to do well six weeks after her original surgery, tolerating serial expansion well
(Figure 10).
After expansion is completed, the goal is to exchange the TEs for permanent silicone gel implants after consolidation and perform a series of revision shaping procedures that will include nipple repositioning and reconstruction. As the patient was found to have early stage breast cancer with no evidence of metastatic disease, she did not need radiation.
Discussion
Our practice’s view is that immediate implant-based reconstruction should benefit from every technique advantage possible given the high stakes of a complication. This extirpative surgical procedure can leave thin or traumatized flaps vulnerable to hypoperfusion. Mastectomy flap necrosis, implant exposure, and deep space infection can be devastating and expensive problems. Successful deployment of an ADM depends on deep ingrowth and incorporation; like other grafts, this depends on proximity to healthy vascularized tissue without infection, fluid collection, or shearing forces.
This case demonstrates the use of the PREVENA RESTOR BELLA•FORM™ System during the crucial immediate and early post-operative period. The unusual circumstances of the case presented an insult to the soft tissue envelope that was greater than normal in a patient with already challenging anatomy.
Kim et al showed that ciNPT applied over incisions reduced wound-related complications and mastectomy flap necrosis in women undergoing immediate expander-based reconstruction.1 Gabriel and colleagues went further and found that patients who received ciNPT over closed incisions following postmastectomy breast reconstruction experienced a shorter time to drain removal and significantly lower rates of infection, dehiscence, necrosis, and seromas, compared with standard-of-care dressings.2 In a separate study of ciNPT after oncological breast surgery, researchers found that ciNPT patients experienced significantly lower postsurgical complication rates (4% vs. 45%) than the standard-of-care group.3
When using the PREVENA RESTOR BELLA•FORM™ System, the benefits of this therapy are applied to an entire area at risk and can potentially help improve outcomes after plastic surgery of the breast. This patient strongly preferred to avoid delay in TE placement if possible, fully informed of the unusual circumstances we faced and the risks of proceeding.
Due to our having access to laser angiography and the PREVENA RESTOR BELLA•FORM™ System, we were confident that proceeding with the selected surgical course was reasonable. Without these tools, we would have closed the patient on postoperative day 1 and delayed her reconstruction. The success of this operation allowed us to avoid additional delays and get the patient on the path to a quicker recovery despite the intraoperative anesthesia-related complication.
Patient data and photos courtesy of Dr. Owen N. Johnson III.
As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
NOTE: Specific indications, contraindications, warnings, precautions and safety information may exist for these products. Please consult a healthcare provider and product instructions for use prior to application. Rx only.
References
Kim DY, Park SJ, Bang SI, Mun GH, Pyon JK. Does the Use of Incisional Negative-Pressure Wound Therapy Prevent Mastectomy Flap Necrosis in Immediate Expander-Based Breast Reconstruction? Plast Reconstr Surg 2016;138(3):558-566. doi:10.1097/PRS.0000000000002431.
Gabriel A, Sigalove S, Sigalove N et al. The Impact of Closed Incision Negative Pressure Therapy on Postoperative Breast Reconstruction Outcomes. Plast Reconstr Surg Glob Open 2018;6(8):e1880.
Ferrando PM, Ala A, Bussone R, Beramasco L, Actis Perinetti F, Malan F. Closed Incision Negative Pressure Therapy in Oncological Breast Surgery: Comparison with Standard Care Dressings. Plast Reconstr Surg Glob Open 2018;6(6):e1732.
©Copyright 2020 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. PRA-PM-US-02477 (05/20).

