Dr. Orgill is Vice Chairman for Quality Improvement in the Department of Surgery at Brigham and Women’s Hospital and Professor of Surgery at Harvard Medical School. He is a reconstructive plastic surgeon and has a PhD from MIT in Medical Engineering. He is the Director of the Brigham and Women’s Hospital Wound Care Center and runs a tissue engineering and wound healing laboratory. His lab at BWH is working to develop better technologies to treat wounds including work with artificial skin, micromechanical forces, platelets, and stem cells. He has consulted for several medical device and start-up companies and is the inventor on several patents. He worked on the team that developed Integra, a skin replacement therapy that has been commercially developed and used successfully on thousands of patients.
Orgill_Current Dialogues in Wound Management_2018_Volume 4_Issue 3
Plastic surgeons have the capacity to transfer large volumes of viable tissue, including skin, to heal virtually every wound. Yet as someone who directs a Wound Care Center, I only use these techniques on a fraction of patients that I see. Most wounds will heal with simpler methods and surgery carries substantial risks.
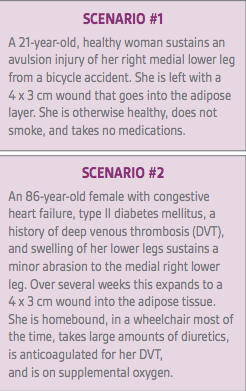
We all know of conditions that delay wound healing: age, smoking, steroid medications, malnutrition, and peripheral vascular disease. Some of these conditions are modifiable, and some are not. Clearly correcting as many risk factors that slow wound healing is essential as a first step. Beyond this, there are personal desires and goals that should be taken into account when selecting therapies. Consider the following two scenarios:
In both cases, these patients have wounds of similar dimensions and anatomic locations yet the treatment and approach to these patients is likely to be substantially different. In both cases, the goals, risks, benefits, and alternative potential treatments need to be explored and discussed with patients. As there are over 1,500 wound care products available in the US market and numerous surgical procedures that could be considered, these can be complex decisions.
Both patients would ideally like rapid healing that leaves no scar, causes minimal pain, is low cost, and is without activity constraints. Unfortunately, there are no products or procedures that that will accomplish all of these goals. Therefore, the wishes of each patient need to be prioritized, and compromises will need to be made.
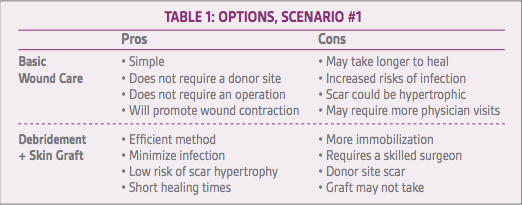
In scenario #1, after discussion, the long-term appearance of her leg is the most important factor for her. She is willing to undergo staged procedures to try and optimize the appearance. She could be offered basic wound care that will allow the wound to heal over a few weeks with potential scar revision several months later. As she is young and healthy, this wound will likely heal without the need for advanced wound care products. Alternatively, she could be offered surgical debridement with a skin graft immediately to expedite healing. To allow her to continue to ambulate some, this could be affixed with a negative pressure wound therapy device. A full-thickness graft from a concealed area such as the groin will minimize donor site scarring concerns. This approach will allow for a faster healing but will leave her with a depressed area in her lower leg that she could elect to have revised in the future. She would need to weigh the pros and cons of each approach to help in her decision (Table 1).
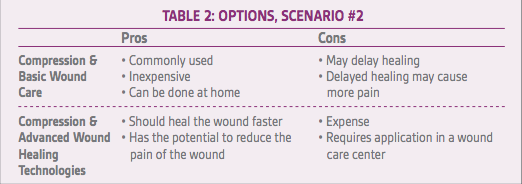
In contrast, the conversation in scenario #2 would be quite different. In this case, her main complaint is the pain the wound causes. Because of her congestive heart failure, she is not an ideal surgical candidate, and surgery would only be considered, if her health improved and other methods fail. A number of advanced wound care technologies such as bioengineered skin substitutes and placental derived constructs could be considered as well as standard compression based dressings. She dislikes compression, but understands that without it, none of the options discussed will work over the long term. After discussion,
we narrow options to standard compression therapy and standard compression therapy plus an advanced wound care modality.
Comparing the pros and cons of Scenario #2, it becomes apparent how to focus the discussion on her goals (Table 2). For example, if she feels she is nearing the end of her life and doesn’t want to be bothered going to a lot of physician appointments, standard dressing care may have an advantage. Many patients are responsible for high co-pays and deductibles depending on their insurance carrier. Trying to help her understand exactly how much advanced treatments cost may help her make informed value decisions. As with Scenario #1, wound debridement and a skin graft is something she may ask about. If surgery were to be considered, she would have to be compliant with leg compression and her anticoagulation would need to be adjusted in the perioperative period.
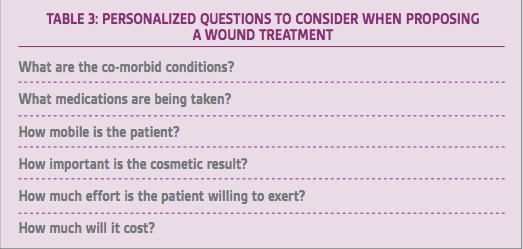
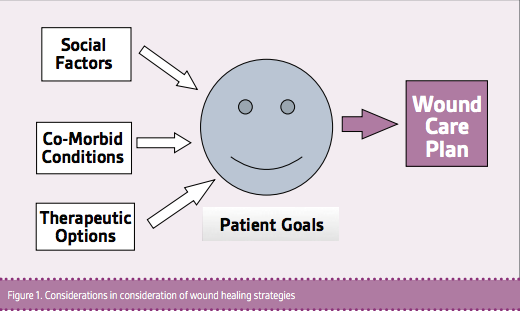
In summary, for seemingly similar wounds, the approach to wound care and possible surgery can be dramatically different depending on the specific patient. Understanding the medical history, the risks and benefits of each potential therapy, and the goals of the patient are essential in weighing the tradeoffs of each therapy (Table 3 and Figure 1).