Dr. Shaw graduated from Albright College in Reading, Pa. with a bachelor of science and a medical degree from Des Moines University in Des Moines, Iowa. He is board certified and a fellow in emergency medicine, He is also a fellow of the American Board of Wound Healing.
Today, Dr. Shaw is a medical director and full time clinician at the Mount Nittany Center for Wound Care in State College, Pa. with extensive experience in epidermal grafting having performed over 400 procedures. He currently functions as a consultant, national/regional speaker and advisory board member for the Acelity corporation.
Shaw_Advanced Wound Dressings Today_2017_Spring Supplement
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
By: Mark R. Shaw, DO, FACEP, FAPWCA
Today, after more than 400 epidermal grafts performed at our wound center, this procedure has become the treatment of choice in our center for the final closure of wounds and ulcers when indicated. With a success rate above 90%* we have learned a few things that help to make that a reality. Essential to that outcome is wound bed preparation.
Wound bed preparation is defined as “the management of the wound to accelerate endogenous healing or to facilitate the effectiveness of other therapeutic measures.” There are multiple factors that will ultimately affect the outcome of wound healing. Each one of these has to be appropriately addressed and managed in order to develop a wound bed that is adequately prepared for epidermal grafting. Not to ignore anyone of these elements; it has been our experience that there are 4 primary factors that have demonstrated the highest incidence for graft success. They are: 1.Recognition of adequate blood flow2.Development of an appropriate granulation wound bed 3.Infection control4.Chronic inflammation managementPrimary attention to these along with other exogenous factors will go a long way to achieving the ultimate result of closure.
All patients need appropriate vascular screening to assure that adequate oxygen at the tissue level is present. Patients with lower extremity wounds should have initial ankle brachial index evaluations for this purpose regardless of the type of wound being managed. If results indicate an increased probability of vascular insufficiency arterial duplex ultrasonography is performed and the patient sent for vascular consultation. If indicated, revascularization is performed prior to grafting. In our experience arterial ulcerations have the highest incidence of graft failure. Recognition and treatment therefore becomes essential in this class of wound.
An adequate granulation bed is the foundation needed for epidermal graft placement. It must be void of eschar, thick fibrinous exudate such as slough and necrotic tissue. Sequential sharp surgical debridements are paramount in meeting this end. This is performed on a weekly basis until only granulation tissue is present. Keep in mind that gentle management of tissues during this process will maintain and enhance neovascularization, the literal lifeblood of the graft. If the patient is unable to tolerate this form of debridement or an existing coagulopathy prohibits it, enzymatic debridement is a viable alternative. Ideally, all tendon or bone should be covered. Improving the wound depth is required to obtain a reasonable cosmetic outcome. Control of wound depth in many cases can be best managed with NPWT. Ultimately developing a depth of 2 mm or less prior to graft application will limit the deformity created by healing over an untoward cavitation.
Infection control requires early recognition and diagnosis. Obtaining a proper wound culture is the first step in this process. A deep tissue source following debridement is critical in evaluating the wound for an acute infection. Targeted antibiotic therapy can then proceed. The eradication of an active infection will reduce the significant potential for graft failure. We recommend a minimum of 2 weeks of treatment prior to grafting. Obviously, this can be longer when IV therapy or when multi organism infection control is required. When a wound has developed a state of persistent inflammation a graft failure is almost assured. When a potential wound for grafting demonstrates this stalled status (no change in status over 2-4 weeks), one such cause can be increased activity of the inflammatory cells. We now use collagen with ORC as a primary dressing for 2 weeks prior to grafting in all patients. We believe that this helps to promote the progression of the wound from the inflammatory to the proliferative stage of wound healing which is more receptive to receiving an epidermal graft.
In order to help elucidate this process of wound bed preparation for epidermal grafting the following two clinical cases give a very good representation of affective outcomes when the factors that affect wound healing are controlled and appropriate interventions utilized.
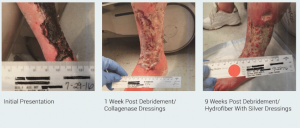
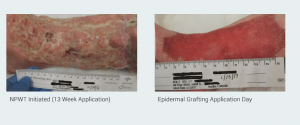
CASE 1
This case involves a 66 F with extensive tissue loss of the left lower extremity due to arterial ulcerations in the face of significant PVD. This patient has multiple co-morbid conditions including CAD, hypertension and a prior failed fem-pop bypass graft. She is still under our care having just received her first two staged epidermal grafts. Her treatment in the clinic has encompassed 6 months of therapy including surgical debridement, collagenase dressing, NWPT, IV and oral antibiotic therapy and endovascular revascularization.
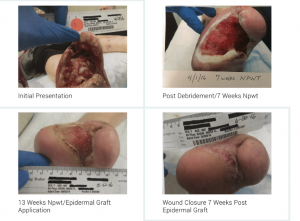
CASE 2
This case involves a 67 F who underwent a trans-metatarsal amputation of her left foot and additional surgical debridement for osteomyelitis and necrotizing fasciitis/gas gangrene. This patient has significant co-morbid conditions that consist of diabetic neuropathy, PVD, hypertension, hypothyroid disease and nicotine addiction. Her treatment in the clinic included surgical debridement, NWPT (13 weeks), HBO (60 treatments), IV and oral antibiotic therapy and epidermal grafting to closure.
CONCLUSIONS
In our opinion, epidermal grafting, in its current state, is becoming more and more recognizable as the standard of practice for the final closure procedure of any wound or ulcer. Its ease of application, patient safety, patient convenience and excellent closure results will continue to help it grow in acceptance.
Success in accomplishing an effective outcome is directly linked to an adherence of definable and replicable practice techniques. Wound selection, management of both endogenous and exogenous factors and appropriate epidermal grafting application with ongoing wound management are all final elements needed to complete this task.
As demonstrated, effective wound bed preparation enables even the most complicated wounds to close. Focus on having adequate blood flow, wound bed granulation, infection control and management of chronic inflammation satisfy a valuable link in the chain of success for wound closure with epidermal grafting.
References
1.Mount Nittany Center for Wound Care, State College, Pa.
2.Schultz GS, Sibbald RG, Falanga V et al. Wound bed preparation: a systematic approach to wound management. Wound Repair Regen. 2003;11(Supp 1):S1-S28