Dr. Allen Gabriel is a member of the American Society of Plastic Surgeons and in 2001, Dr. Gabriel was chosen by the prestigious Loma Linda University to join the Integrated Plastic Surgery Residency Program. While at Loma Linda University, he volunteered on a medical mission to Ethiopia with Operation Good Samaritan. In addition, he served on several leadership committees and was the chief resident prior to completing his residency. In 2007, Dr. Gabriel was selected by world-renowned plastic surgeon Dr. G. Patrick Maxwell to enter a Breast and Aesthetic Surgery Fellowship in conjunction with Baptist Hospital in Nashville, Tennessee. Completion of this program provided him with advanced training in breast and aesthetic surgery.
Dr. Gabriel is one of the few medical students in the country to have received the prestigious Humanism in Medicine Award. This award lead to the creation of the University of Nevada’s Humanism in Medicine Honor Society, of which Dr. Gabriel is still an active member. During medical school, he was involved with both clinical and basic science research, earning several research awards and publications prior to graduating. Dr. Gabriel is board certified in plastic surgery and has been invited to speak nationally and internationally on breast and aesthetic surgery.
Gabriel and Rice_Innovations in Addressing Non-Viable Tissue_2018_Volume 1_Issue 1
INTRODUCTION
Over the last few years, advancements in negative pressure wound therapy (NPWT) with instillation have made the system easier to use. The first commercially available instillation system (V.A.C. INSTILL™ Wound Therapy System) used timed, intermittent, gravity-fed delivery of an instilled topical wound solution in conjunction with NPWT and demonstrated positive clinical outcomes in a variety of acute and chronic wounds.1-5 To further simplify and enhance the precision of this instillation technique, a next-generation device was developed that automated and volumetrically controlled the delivery of topical solutions to the wound bed with a user-selected dwell time, followed by removal of the topical solution via NPWT. Additionally, specialized dressings were designed to be used specifically with NPWT with instillation and a dwell time (NPWTi-d).6,7 Since its inception, there have been several recommendations and guidelines published8-11 as well as numerous studies on the use of NPWTi-d for the management of complex wounds.
More recently, a novel reticulated open cell foam dressing with through holes (ROCF-CC; V.A.C. VERAFLO CLEANSE™ CHOICE Dressing) has been developed that assists with wound cleansing by removing thick wound exudate and devitalized tissue in patients when debridement is not possible or appropriate. A recent retrospective case series by Teot et al17 was the first to report on the use of NPWTi-d with ROCF-CC for patients with complex wounds containing areas of devitalized tissue. Their preliminary results suggested that “adjunctive use of NPWTi-d with ROCF-CC may help clean large, complex wounds when complete surgical debridement is not possible or appropriate and/or when areas of slough and non-viable tissue remain present on the wound surface.”17 We report on our initial experience using NPWTi-d with ROCF-CC on a patient with complex wounds.
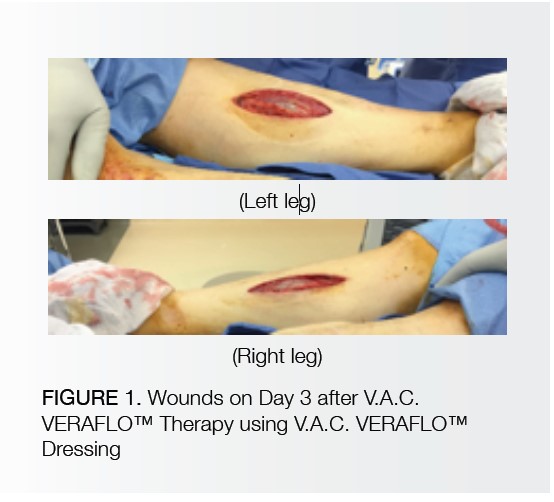
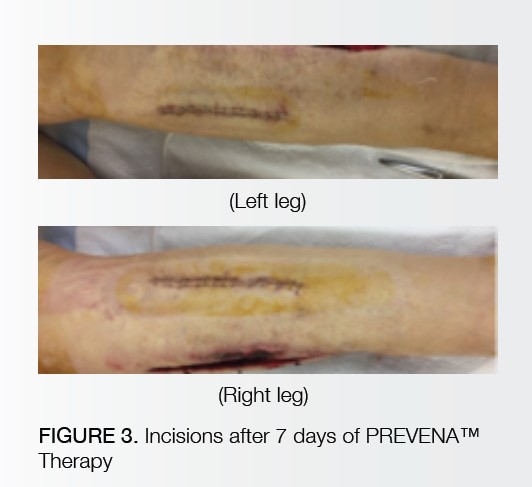
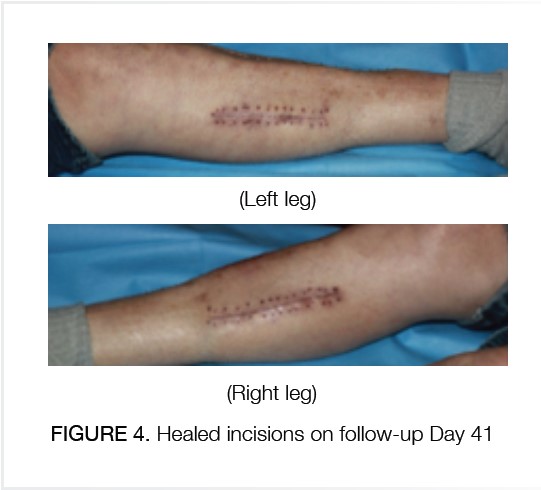
A 65-year-old male with a history of coronary artery disease, peripheral vascular disease, hypertension, and diabetes underwent open abdominal aortic aneurysm repair with a clamp time of less than 2 hours. The patient subsequently developed bilateral lower extremity compartment syndrome and underwent open fasciotomies. Following one debridement and wet-to-dry dressing changes, the plastic surgery department was consulted. At this time, another debridement was performed to remove necrotic muscle, and V.A.C. VERAFLO™ Therapy using the V.A.C. VERAFLO™ Dressing was initiated for 3 days using instillation of saline with a 1-second dwell time, followed by 2 hours of NPWT (-125 mmHg) (Figure 1). The dressing was switched to V.A.C. VERAFLO CLEANSE CHOICE™ Dressing, and therapy resumed using the same therapy settings. On Day 7, the wounds were surgically closed, and the PREVENA™ Incision Management System was applied to the closed incisions (Figure 2). After 7 days, the PREVENA™ Incision Dressing was removed from the incisions (Figure 3). At follow-up Day 41, both incisions remained healed (Figure 4).
DISCUSSION
Given the complex nature of this case, advanced therapies and surgical principles were utilized to achieve final closure of the wounds. However, the large amount of muscle loss from the different compartments made it difficult to determine what type of closure would be achieved. One option would have been to continue with wet-to-dry dressing changes, which would have taken a prolonged period of time and potentially increased the pain and discomfort for the patient during the dressing changes. The next option was utilizing standardV.A.C.® Therapy (-125 mmHg); however, this would not have given us the cleansing that was needed for this type of wound. One other option was available that provided the necessary wound cleansing along with application of negative pressure, V.A.C. VERAFLO™ Therapy. The cleansing benefit of V.A.C. VERAFLO™ Therapy has been described in other published studies12,13,15,16 and consensus/recommendation guidelines.8-10 Our goal is always to cleanse and cover the wound by the most efficient means and having access to V.A.C. VERAFLO™ Therapy gives us the opportunity to achieve this goal.
In this particular case, we found that: •early utilization of V.A.C. VERAFLO™ Therapy was critical•V.A.C. VERAFLO™ Therapy cleansed the wound•NPWT during V.A.C. VERAFLO™ Therapy reduced edema to help achieve delayed primary closure•V.A.C. VERAFLO CLEANSE CHOICE™ Dressing assisted in removal of non-viable tissue and enhanced cleansing•PREVENA™ Therapy assisted in healing of the delayed primary closure incisions
This case is a perfect example of what appropriate adequate debridement followed by instillation therapy in combination with NPWT can provide. The goal of any wound is to achieve closure in an efficient manner. In this case, a delayed primary closure instead of a skin graft was a much better option for the patient. Hypothetically, if full granulation was achieved by whichever modality described, then complete closure would have been accomplished with a split-thickness skin graft. The aggressive early management with V.A.C. VERAFLO™ Therapy and starting the closure process early was the key to the success of a delayed primary closure.
References
1.Bernstein BH, Tam H. Combination of subatmospheric pressure dressing and gravity feed antibiotic instillation in the treatment of post-surgical diabetic foot wounds: A case series. Wounds 2005;17:37-48.
2.Gabriel A, Shores J, Heinrich C et al. Negative pressure wound therapy with instillation: a pilot study describing a new method for treating infected wounds. Int Wound J 2008;5:399-413.
3.Wolvos T. Wound instillation – The next step in negative pressure wound therapy. Lessons learned from initial experiences. Ostomy Wound Manage 2004;50:56-66.
4.Schintler MV, Prandl EC, Kreuzwirt G, Grohmann MR, Spendel S, Scharnagl E. The impact of V.A.C. Instill in severe soft tissue infections and necrotizing fasciitis. Infection 2009;37:31-32.
5.Raad W, Lantis JC, II, Tyrie L, Gendics C, Todd G. Vacuum-assisted closure instill as a method of sterilizing massive venous stasis wounds prior to split thickness skin graft placement. Int Wound J 2010;7:81-85.
6.Gabriel A, Kahn KM. New advances in instillation therapy in wounds at risk for compromised healing. Surgical Technology International2014;24:75-81.
7.Gabriel A. Integrated negative pressure wound therapy system with volumetric automated fluid instillation in wounds at risk for compromised healing. Int Wound J 2012;9:25-31.
8.Kim PJ, Attinger CE, Steinberg JS et al. Negative-Pressure Wound Therapy with Instillation: International Consensus Guidelines. Plast Reconstr Surg 2013;132:1569-1579.
9.Kim PJ, Attinger CE, Crist BD et al. Negative pressure wound therapy with instillation: review of evidence and recommendations. Wounds2015;27:S2-S19.
10.Gupta S, Gabriel A, Lantis J, Teot L. Clinical recommendations and practical guide for negative pressure wound therapy with instillation. Int Wound J 2016;13:159-174.
11.McKanna M, Geraci J, Hall K et al. Clinician panel recommendations for use of negative pressure wound therapy with instillation. Ostomy Wound Manage 2016;3-14.
12.Gabriel A, Kahn K, Karmy-Jones R. Use of negative pressure wound therapy with automated, volumetric instillation for the treatment of extremity and trunk wounds: clinical outcomes and potential cost-effectiveness. Eplasty 2014;14:e41.
13.Brinkert D, Ali M, Naud M, Maire N, Trial C, Teot L. Negative pressure wound therapy with saline instillation: 131 patient case series. Int Wound J 2013;10:56-60.
14.Fluieraru S, Bekara F, Naud M et al. Sterile-water negative pressure instillation therapy for complex wounds and NPWT failures. J Wound Care 2013;22:293-299.
15.Kim PJ, Attinger CE, Steinberg JS et al. The impact of negative-pressure wound therapy with instillation compared with standard negative-pressure wound therapy: a retrospective, historical, cohort, controlled study. Plast Reconstr Surg 2014;133:709-716.
16.Kim PJ, Attinger CE, Oliver N et al. Comparison of Outcomes for Normal Saline and an Antiseptic Solution for Negative-Pressure Wound Therapy with Instillation. Plast Reconstr Surg 2015;136:657e-664e.
17.Teot L, Boissiere F, Fluieraru S. Novel foam dressing using negative pressure wound therapy with instillation to remove thick exudate. Int Wound J 2017.